Health care systems are complex, high-risk environments. Medical knowledge is expanding exponentially and producing data about health care delivery. Health systems research enhances our understanding of system-level improvements and innovations and seeks to identify factors influencing care delivery.
R&E Military Health System Research supports the Military Health System, one of America's largest and most complex health care systems, which serves approximately 9.6 million beneficiaries. MHSR uses data to tease out patient-, system-, regional- and facility-level variables that can influence outcomes and improve beneficiary health. These efforts lead to military health care that is safe, effective, accessible and patient-centered.

MHSR is key to ensuring the evolution of the Military Health System into a high-reliability organization skilled at acquiring and transferring knowledge and using new knowledge and insights to modify behaviors. As a strategic project in the DHA FY22-26 Campaign Plan, MHSR is a vital tool for generating critical evidence and actionable insights about health economics/costs, quality, variation, outcomes, health system reform, and health readiness.
Annual MHSR Grant Program
The MHSR program supports research projects with potential to innovate and improve military health care through annual grant awards. Funding for MHSR grants is made available through the Defense Health Program. For each funding round, MHSR publishes a Notice of Funding Opportunity on grants.gov seeking rigorous intramural and extramural health systems research based on MHSR and clinical research priorities. The process for soliciting and reviewing proposals and awarding grants is updated each year.
The Fiscal Year 2025 Notice of Funding Opportunity for MHSR grants is expected to be released in February 2024.
MHSR Grant Process
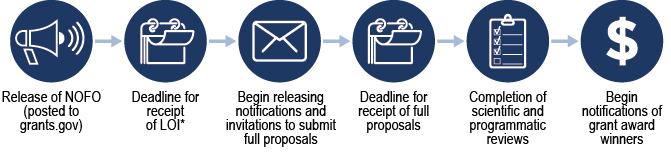
*LOI: Letter of Intent
MHSR Priority Topic Areas and Clinical Priority Areas
Proposed research must address at least one MHSR priority topic area and one MHSR clinical priority area. Letters of Intent applicants that do not meet this requirement will not be asked to submit a full proposal.
MHSR Priority Topic Areas:
Economics and Cost – Research on the factors that shape the MHS cost, drive demand and utilization, and influence cost in either TRICARE direct or Click to closePurchased CareThe TRICARE Health Program is often referred to as purchased care. It is the services we “purchase” through the managed care support contracts.purchased care systems; issues related to efficiency, effectiveness, value and behavior in the production, and utilization of health care in terms of costs, charges, and expenditures; the impact of technologies on care delivery and cost; and the impact of workforce, recruitment, and retention of medical personnel. Research that delineates value-based care within the MHS in both purchased and Click to closeDirect CareDirect care refers to military hospitals and clinics, also known as “military treatment facilities” and “MTFs.”direct care; pre- and post- studies to evaluate the impact of the structure of the TRICARE contract on patient care.
Quality – Research which examines the degree to which health services for individuals and populations are safe, effective, patient-centered, timely, efficient, and equitable with the outcome of increasing the likelihood of improved health. The impact of standardizing clinical practice through clinical practice guidelines, evidence-based practices, and process improvements, on the health of the population/sub-population.
Outcomes – Health outcome research identifies and measures the factors which impact a population of patients at the enterprise, geographic market level, or sub-population levels; examines the system level factors which influence achievement of the Quadruple Aim “better health” in comparison to private sector efforts. Health outcomes research incorporates clinical outcomes, financial impact, patient health, quality of life, and measurement of indicators that predict results important to patients and patient experience.
Variation – Studies that examine the factors that influence unwarranted variation or differences in quality, utilization, cost, or outcomes within the MHS and the implications to the enterprise as a system of system of care.
Health Readiness – Burden of disease and associated health and risk factors within the MHS populations that affect active-duty service members’ ability to deploy. Implications of disease burden as an indicator of medical readiness, potential impact to staffing, network utilization, and cost for direct care and/or purchased care.
Health System – Research related to the impact of the significant changes in policy or structure of the MHS on health care cost, quality, utilization, health outcomes, manpower/staffing, or health care readiness. Comparisons between direct and purchased care, or care within the private sector, and includes measurement of the impact of policy changes to the TRICARE benefit structure on utilization and cost.
FY2025 MHSR Clinical Priority Areas (new areas are determined each grant cycle):
- Behavioral Health
- Neuro-musculoskeletal
- Primary Care
- Specialty Care
- Surgical Services
- Women and Infant
- Telehealth
- Dental
Helpful Resources
For Health Services Research Funding and Resources
For the Military Health System
For Researchers Concerning Data and Data Sharing
Fiscal Year 2023 MHSR Research Awardees
| Institution |
Project Title |
| USU/HJF |
Impacts of TRICARE's Expansions of Behavioral Health Benefits and Provider Availability on Access to and Utilization and Expenditure of Behavioral Health Care, Health Outcomes, and Medical Readiness |
| Complex Ped/Geneva |
Health Care Transitions for Military-Connected Children and Spouses with Complex Medical Conditions |
| USU/HJF |
Improving healthcare value and access for mother-infant dyads in the Military Health System: complex care co-location, transfer patterns, and service quality |
| USU/HJF |
Assessing the Effect of the Military Health System Consolidation under a Single Management Structure on Health Care Utilization, Cost, Quality and Military Readiness |
| USU/HJF |
Impact of the COVID-19 Pandemic on Rehabilitation Care Utilization and Delivery for Active-Duty Service Members with Neuromusculoskeletal Injuries |
| Defense Health Management Systems/HJF |
Contraceptive Care among Active-Duty Service Women |
| UARIEM |
Service-member Post-Operative Rehabilitation and Training to Improve Outcomes, Optimize Military Return-To-Duty, and Mitigate Re-Injury and Lower Extremity after Lower Extremity Surgery |
| Penn State |
Direct vs. Purchased Care as Drivers of Geographic Variation in Cancer Outcomes in the Military Health System |
Fiscal Year 2022 MHSR Research Awardees
| Institution |
Project Title |
| Cornell University |
Efficiency of Direct vs Purchased Care Primary Care Managers |
| USC |
The Cost Effectiveness and Value of Treating Combat Ocular Trauma |
| Dartmouth Hitchcock Medical Center |
Quality of Care for Children With Medical Complexity in the Military Health System and Association With Maternal Behavioral Health |
| VA Boston Healthcare System |
Enhancing Measurement-Based Behavioral Health Care in the Military Health System |
| Trustees of Dartmouth College |
Understanding Market Determinants of Variation: Using compulsory Migration to Study Variation in Spending and Utilization |
| UMD School of Medicine, Baltimore |
Value-based Military Sleep Medicine: Health Economic Aspects of Sleep Disorders Treatments in the US MHS |
| USUHS |
Medical READiness PROject (MED READ PRO) |
| Naval Health Research Center |
Navy Medicine's Temporary Limited Duty Patient Population: Evidence about Care Source and Case Management Services to Inform the MHS |
| NICoE/ WRNMMC |
Recovery Expectations in TBI Related Outpatient Settings: Identifying key trajectories of recovery in service members and veterans |
| USA Medical CoE/ BAMC |
The Effects of Nursing Staff Mix and Turnover on Productivity and Outcomes |
| Naval Health Research Center |
Patterns of Tele-Behavioral Health Care Utilization Among Active Duty Service Members Across |
USA Research Institute of
Environmental Medicine |
Examining the Role of Social Networks on Health-Related Behaviors and Musculoskeletal-Related Medical Discharges in the Army |