Abstract
This report presents the incidence and prevalence of diagnosed female infertility among active component service women. During 2013–2018, 8,744 active component women of childbearing potential were diagnosed with infertility for the first time, resulting in an overall incidence of 79.3 cases per 10,000 person-years (p-yrs). Compared to their respective counterparts, women in their 30s, non-Hispanic blacks, those in health care and pilot/air crew occupations, Army personnel, and those who were married had the highest incidence rates. The incidence of diagnosed female infertility decreased from 85.1 per 10,000 p-yrs in 2013 to 63.6 per 10,000 p-yrs in 2018 despite a concurrent increase in the rate of fertility testing. During the surveillance period, the average annual prevalence of diagnosed female infertility was 1.6%. Of the service women who were diagnosed with infertility for the first time during the surveillance period, 1,808 (20.7%) delivered a live birth within 2 years after the incident infertility diagnosis. Current findings indicate that the prevalence of diagnosed female infertility among active component service women is lower than estimates of self-reported infertility from surveys of U.S. civilians and service women.
What Are the New Findings?
The prevalence of diagnosed infertility among female active component service members is low compared to estimates of self-reported infertility obtained from U.S. national and military surveys. The incidence of diagnosed female infertility decreased between 2013 and 2018 despite a concurrent increase in the rate of fertility testing.
What Is the Impact on Readiness and Force Health Protection?
Although the incidence, prevalence, and burden of diagnosed infertility among active component service women are relatively small, there are some subgroups of women who are at higher risk. It is important to identify the underlying physical cause of infertility in order to administer proper treatment and prevent additional sequelae.
Background
Clinical infertility is the failure of a woman of childbearing age to become pregnant after 1 year of regular, unprotected sexual intercourse.1 The reasons for infertility can involve 1 or both partners, but in some cases no cause can be identified. Ovulation disorders are estimated to account for one-third of infertility cases, and they often present with irregular periods (oligomenorrhea) or the absence of periods (amenorrhea).2 The most common cause of infertility related to anovulation is polycystic ovary syndrome, a hormone imbalance that can prevent the ovaries from releasing eggs.3 Other causes of infertility include fallopian tube damage or blockage, uterine or cervical abnormalities, hypothalamic-pituitary hormone imbalances, endometriosis, and primary ovarian insufficiency (i.e., premature Click to closemenopauseA point in time 12 months after a woman's last period. This transitional period begins between ages 45 and 55.menopause).3
Tubal infertility from blocked or swollen fallopian tubes can be caused by previous sexually transmitted infections (STIs), pelvic inflammatory disease (PID), or history of a ruptured appendix or abdominal surgery.1 Uterine or cervical abnormalities include structural abnormalities or the growth of benign tumors called fibroids, which can interfere with the passage and implantation of the fertilized egg within the Click to closeuterusAlso known as the womb, the uterus is the female reproductive organ where a baby grows. uterus.1 Hypothalamic-pituitary hormone imbalances such as hypogonadotrophic hypogonadism can be caused by excessive exercise, being underweight, or both.2 Endometriosis occurs when endometrial tissue implants and grows outside of the uterus, affecting the function of the female genital organs.4 Causes of premature menopause can include genetic disorders, immunological and metabolic disorders, smoking, and use of chemotherapeutic drugs.5
Because ovarian function as well as the number and quality of eggs released decreases with advancing age, age may be an increasingly important factor contributing to rates of infertility in the U.S., as many women are delaying pregnancies to their 30s and 40s. In 2017, approximately 10% of all firstborn children in the U.S. were born to women aged 35 years or older, and about one-third were born to women aged 30 years or older.6 This trend has also been observed among women serving in the U.S. military. Among female service members, the highest live birth rates during 2012–2016 were observed among women aged 30–34 years, and the prevalence of pregnancy among women aged 35–39 years increased from 10.7% in 2012 to 11.7% in 2016.7
In 2018, the Service Women's Action Network (SWAN) conducted an online survey focused on reproductive health services in the military. Of the 799 total survey Of the active duty service women who answered questions about infertility, 37% said that they had trouble getting pregnant when actively trying to do so.8 The results of this survey caused concern among military leadership, as the findings suggested a much higher prevalence of female infertility among service women compared to the Centers for Disease Control and Prevention's (CDC's) national prevalence estimate. According to the CDC's 2011–2015 National Survey of Family Growth, the prevalence of infertility among married women 15–44 years old was 6.7%; 12.1% of women aged 15–44 years reported impaired fecundity.9 The CDC defined infertility as a self-report of at least 1 year of failed attempts for married/cohabitating partners at getting pregnant when neither the respondent nor her current husband/cohabiting partner was surgically sterile and when the couple had been sexually active each month without contraception.9 Impaired fecundity was defined as self-reported problems getting pregnant and carrying a baby to term regardless of marital/cohabitating status.9 It has been suggested that service women may be at increased risk for infertility because of exposures to environmental toxins as well as traumas and/or stressors experienced during deployments.8,10,11 In addition, relatively higher levels of tobacco use, alcohol use, and PID also may put service women at greater risk for infertility than the national female population.12–14
This report estimates the incidence, prevalence, and burden of medical encounters due to diagnosed infertility among active component service women in the U.S. Armed Forces between 2013 and 2018.
Methods
The surveillance period was 1 Jan. 2013 through 31 Dec. 2018. The surveillance population consisted of all active component service women of childbearing potential who served in the Army, Navy, Air Force, or Marine Corps at any time during the surveillance period. Women of childbearing potential were defined as women aged 17–49 years without any history of Click to closehysterectomyA partial or total surgical removal of the uterus. It may also involve removal of the cervix, ovaries, Fallopian tubes, and other surrounding structures. hysterectomy or permanent sterilization. History of hysterectomy and/or permanent sterilization was defined by having a qualifying diagnostic or procedural code for hysterectomy or permanent sterilization in any position of an inpatient or outpatient record. These diagnostic and procedural codes have been previously described.7,15 All data used for the analyses were abstracted from records routinely maintained in the Defense Medical Surveillance System (DMSS) for health surveillance purposes.
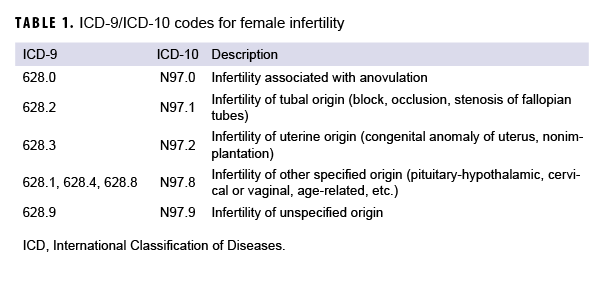
An incident case of infertility was defined by having at least 2 outpatient medical encounters with an infertility diagnosis (International Classification of Diseases, 9th Revision [ICD-9] code 628.*; International Classification of Diseases, 10th Revision [ICD-10] code N97.*) in the first or second diagnostic position or by having an inpatient encounter with an infertility diagnosis in the first diagnostic position. An individual could be counted as a case of infertility only once. The incident date was the date of the first qualifying medical encounter. The type of infertility (anovulation, tubal origin, uterine origin, other, or unspecified) was assigned according to the most specific type that was diagnosed in any inpatient or outpatient encounter record during the case's military service (Table 1). Anovulation was considered the most specific type, followed by tubal origin, uterine origin, other, and unspecified.
For incidence calculations, person-time was censored at the time of the first hysterectomy or permanent sterilization diagnosis, when the service member turned 50 years old, or at the time of the first infertility diagnosis, whichever came first. Person-time for prevalent cases and for women not of childbearing potential was removed from the study population. Incidence was calculated per 10,000 person-years (p-yrs).
To be counted as a prevalent case of infertility, the woman of childbearing potential had to 1) be in active component military service during the calendar year of interest, 2) qualify as an incident case of infertility in the year of interest or any year prior (including before 2013), and 3) have an inpatient or outpatient encounter for any infertility type in any diagnostic position during the year of interest. The denominator for prevalence calculations was the total number of women of childbearing potential in active component service during that year. Prevalence rates were calculated per 10,000 persons.
The burden of medical encounters for infertility was analyzed by calculating the total number of inpatient and outpatient encounters with a primary diagnosis of infertility among all active component service women (including both prevalent and incident cases of infertility). The total numbers of individuals affected and the total number of hospital bed days for infertility were also calculated according to standard MSMR burden methodology.16
To assess the impact that fertility testing may have had on incidence of diagnosed infertility, the rate of fertility testing among all active component women (not just women of childbearing potential) was measured during the surveillance period. Fertility testing was defined by the presence of an inpatient or outpatient encounter with a diagnosis of fertility testing (ICD-9: V26.21; ICD-10: Z31.41) in any diagnostic position. One test per person per day was counted. The denominator was person-time for all female active component service members during the surveillance period.
Finally, incident infertility cases were followed for up to 2 years to measure subsequent live birth deliveries. Live birth deliveries were defined by having a hospitalization with a live birth delivery-related diagnosis (ICD-9: V27* [excluding V271, V274, V277] and ICD-10: Z37* [excluding Z371, Z374, and Z377]) in any diagnostic position.
Results
Incidence
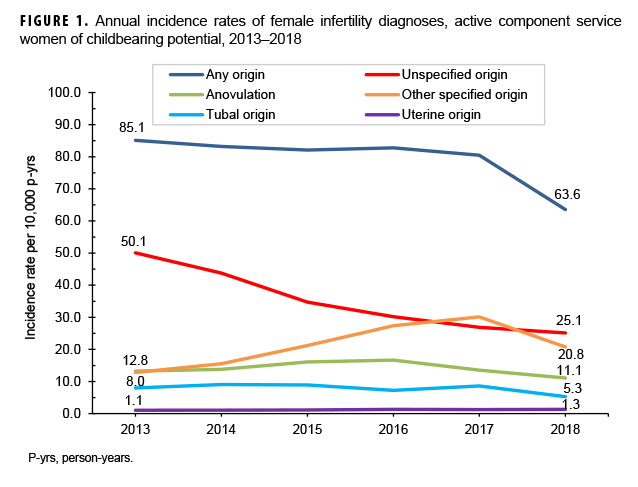
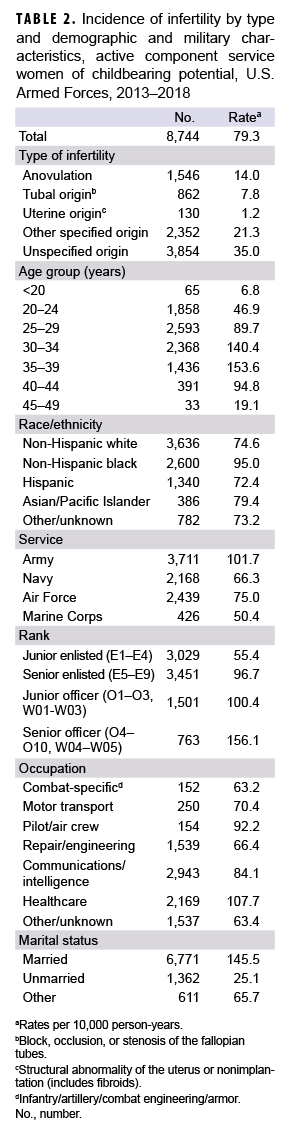
During the surveillance period, 8,744 active component women of childbearing potential were diagnosed with infertility for the first time. The crude overall incidence was 79.3 per 10,000 p-yrs (Table 2). Infertility of unspecified origin was the most commonly diagnosed type (35.0 per 10,000 p-yrs), followed by other specified origin (21.3 per 10,000 p-yrs), anovulation (14.0 per 10,000 p-yrs), tubal origin (7.8 per 10,000 p-yrs), and uterine origin (1.2 per 10,000 p-yrs). Annual incidence rates of diagnosed infertility (of any origin) decreased by 25.3% from 2013 through 2018 mainly because of decreasing rates of infertility of unspecified origin (Figure 1). Incidence of diagnoses of infertility of other specified origins increased between 2013 and 2017 and then dropped in 2018.
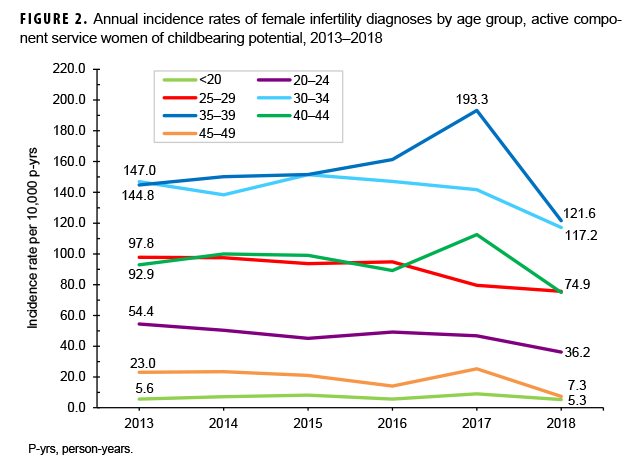
Overall rates of incident infertility diagnoses were highest among women in their 30s and lowest among those in the youngest (<20 years; 6.8 per 10,000 p-yrs) and oldest (45–49 years; 19.1 per 10,000 p-yrs) age groups (Table 2, Figure 2). Annual rates of any infertility diagnosis decreased among service women in all age groups during the surveillance period; however, the smallest decrease occurred among women less than 20 years old (Figure 2). For most age groups, the incidence of infertility diagnosis peaked in 2017.
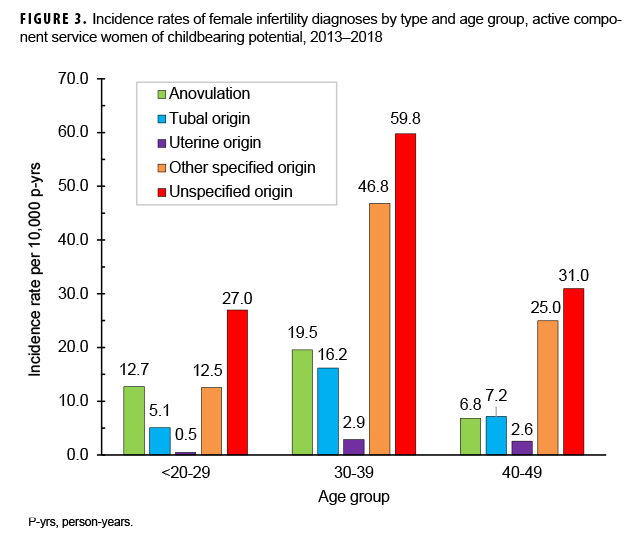
Infertility due to unspecified origin was the most frequently diagnosed type of infertility among service women in all age groups, and infertility of uterine origin was the least frequently diagnosed type (Figure 3). Other specified origin was the next most frequently diagnosed type, except among women in their 20s, for whom the most frequently diagnosed type was anovulation. Among the other 3 types of infertility, anovulation was the most common cause among women under 40 years old. However, infertility due to tubal and uterine origins was more common among women in their 30s and 40s compared to women under 30 years old.
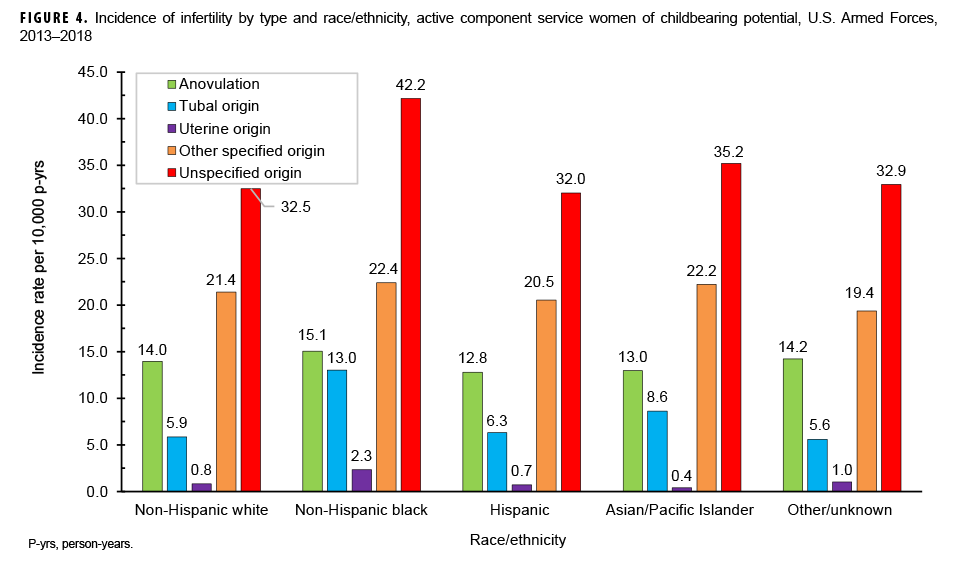
Overall incidence rates of infertility diagnoses of any type were highest among non-Hispanic black service members (95.0 per 10,000 p-yrs) compared to women in other race/ethnicity groups (Table 2). Compared to other racial/ethnicity groups, non-Hispanic black women had the highest rates of diagnoses of all types of infertility (Figure 4).
Overall rates of incident infertility diagnoses were highest among service women in the Army (101.7 per 10,000 p-yrs) and lowest among women in the Marine Corps (50.4 per 10,000 p-yrs) (Table 2). Senior enlisted service women had higher incidence rates than junior enlisted personnel, and senior officers had higher rates than junior officers. Compared to other occupations, service women in health care occupations had the highest incidence of diagnosed infertility (107.7 per 10,000 p-yrs), followed by pilots/air crew (92.2 per 10,000 p-yrs). The rate of incident infertility diagnoses among married service women was nearly 6 times that of unmarried service women and more than twice that of those with "other" marital statuses.
Prevalence
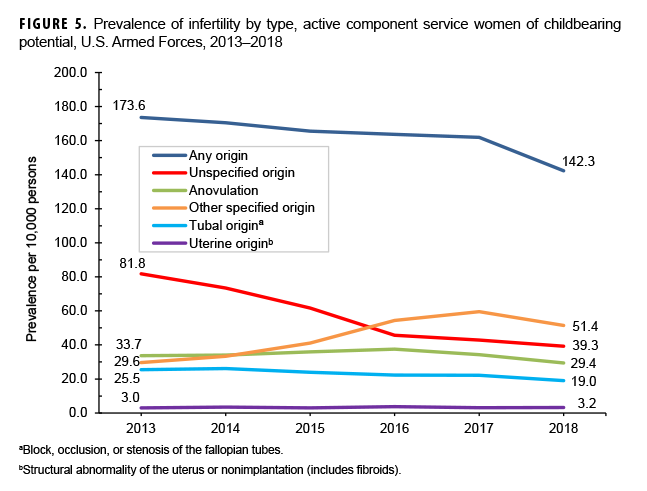
The average annual prevalence of diagnosed female infertility of any type during the surveillance period was 163 per 10,000 persons, or 1.6% (Figure 5). The annual prevalence of all types of diagnosed infertility decreased during the surveillance period, except for infertility of other specified origin, which increased between 2013 and 2017.
Burden
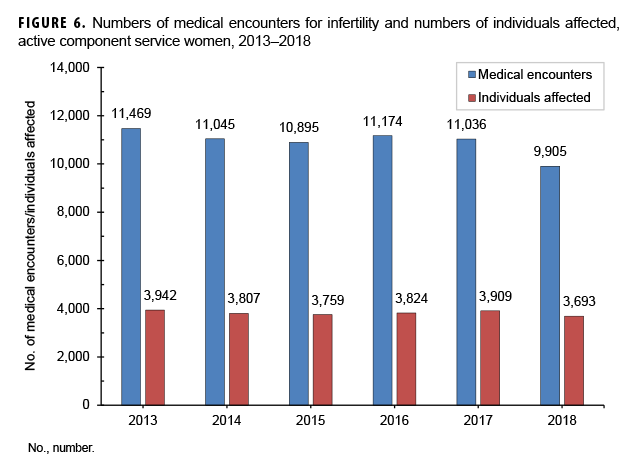
There were 65,524 total medical encounters and 120 hospital bed days for female infertility during the surveillance period (data not shown). Annual numbers of medical encounters during which infertility was reported as a primary (first-listed) diagnoses and the numbers of individuals affected by infertility remained relatively stable during the period (Figure 6). However, the ratio of medical encounters to individuals affected decreased from 2.9 in 2013 to 2.7 in 2018. In 2018, there were 9,892 outpatient encounters for female infertility, which represents 7.3% of all outpatient encounters for conditions affecting the genitourinary system among active component service women in that year (data not shown).17
Fertility testing
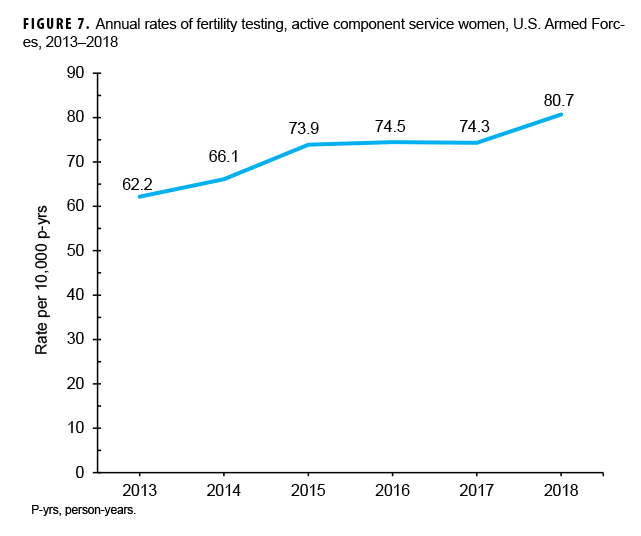
During the surveillance period, annual rates for female fertility testing increased 29.8%, from 62.2 per 10,000 p-yrs in 2013 to 80.7 per 10,000 p-yrs in 2018 (Figure 7).
Live births after infertility diagnosis
Of the 8,744 service women who were diagnosed with infertility for the first time during the surveillance period, 651 (7.5%) had a hospitalization for a live birth within 1 year after the incident infertility diagnosis (data not shown). In total, 1,808 (20.7%) had a hospitalization for a live birth within 2 years after the incident infertility diagnosis.
Editorial Comment
The findings of this report show that the incidence of diagnosed female infertility among active component U.S. service members between 2013 and 2018 was 79.3 per 10,000 p-yrs. The findings also show that rates were highest among women in their 30s and non-Hispanic black women. The most common types of diagnoses of infertility due to specific causes were related to anovulation or of tubal origin. These results are broadly similar to an earlier MSMR analysis of female infertility during 2000–2012.18 Findings from the current analysis show that the overall incidence of diagnosed female infertility decreased between 2013 and 2018 despite a concurrent increase in the rate of fertility testing. In addition, the average annual prevalence of diagnosed female infertility was 163 per 10,000, or 1.6%.
The prevalence of diagnosed infertility among service women from this report (1.6%) is lower than the national self-reported infertility prevalence (6.7%) and much lower than the self-reported estimate among active duty service members in the 2018 SWAN study (37%). Diagnoses of infertility in this report may underestimate the true rate of infertility to the extent that affected service women did not seek care for infertility or sought care outside of the Military Health System. In contrast, the 2018 SWAN study's survey of a nonrepresentative sample of active duty service women likely introduced selection bias in favor of those who had negative experiences related to fertility, which would overestimate the prevalence of infertility.
This report also showed that among women diagnosed with incident infertility, about one-fifth (20.7%) had a live birth within 2 years following the diagnosis. Overall, about 50% of female infertility cases in the U.S. are successfully treated.19 Women with infertility related to ovulation problems are most likely to benefit from treatment. However, successful treatment depends on several factors, including the underlying cause of infertility, age, history of prior pregnancies, and duration of infertility problems. Women in active military service may receive diagnostic services to identify physical causes of infertility and some medically necessary treatments (e.g., hormonal therapy, corrective surgery, or antibiotics).20 However, TRICARE only covers non-coital reproductive therapies (e.g., artificial insemination or in vitro fertilization [IVF]) for service members who lost their natural reproductive abilities because of illnesses or injuries related to active service. Although TRICARE does not cover IVF, there are military treatment facilities that offer low-cost IVF treatment through medical training programs.
Between 2000 and 2012, the highest incidence of infertility among service members was among women aged 30–34 years. However, during 2013–2018, the highest incidence was among women aged 35–39 years, followed closely by women aged 30–34 years. This shift was likely influenced by the increasing rates of clinical care seeking for infertility among women delaying pregnancy until older ages. Similar to the previous report, infertility due to anovulation was more common in younger compared to older age groups, whereas infertility with tubal or uterine origin was more common in older compared to younger age groups. These different distributions of diagnoses in relation to age likely reflect the different pathophysiologic mechanisms associated with various types of infertility.
The finding that the overall incidence of diagnosed infertility was higher among non-Hispanic black service women is consistent with surveillance data indicating a relatively high incidence of risk factors for infertility including STIs, PID, and uterine fibroids among non-Hispanics blacks compared to those in other race/ethnicity groups.13,21,22 Overall incidence was also higher among health care personnel and pilots/air crew. Health care personnel may be more likely to self-diagnose or seek care, which could result in surveillance bias. In contrast, there is some indication that pilots and flight attendants may be at higher risk for reproductive health concerns because of cosmic ionizing radiation, circadian rhythm disruption, and physical job demands.23 Finally, the finding of higher incidence of diagnosed infertility among married service women is likely influenced by greater health care seeking for family planning and even possibly the definition of infertility itself, which the CDC defines as 1 year of failed attempts for married or cohabitating partners at getting pregnant.9
There are several limitations to this analysis. As previously described, diagnoses of infertility may underestimate the true incidence and prevalence of this condition. In addition, the percentage of women who gave birth following incident infertility diagnoses is also likely an underestimate because women who gave birth after leaving military service are not captured. Furthermore, the current analysis did not explicitly capture recurrent pregnancy loss (ICD-9: 629.81, 646.3*; ICD-10: N96, O26.2*), which could be considered a type of infertility. However, some individuals diagnosed with recurrent pregnancy loss may have received a diagnosis of "unspecified infertility" and would have been included in the current analysis.
Despite these limitations, this report provides an update on the incidence and prevalence of diagnosed infertility among active component service women. In contrast to recent survey findings, this report indicates that the incidence and prevalence of diagnosed female infertility are low compared to the self-reported prevalence in the U.S. general population.
References
- Centers for Disease Control and Prevention. Reproductive Health. Infertility FAQs. https://www.cdc.gov/reproductivehealth/infertility/index.htm. Accessed 14 April 2019.
- Hamilton-Fairley D, Taylor A. Anovulation. BMJ. 2003;327(7414):546–549.
- U.S. Department of Health and Human Services. Office of Women’s Health. Infertility. https://www.womenshealth.gov/a-z-topics/infertility. Accessed 14 April 2019.
- Senapati S, Bamhart K. Managing endometriosis-associated infertility. Clin Obstet Gynecol. 2011;54(4):720–726.
- Okeke TC, Anyaehie UB, Ezenyeaku CC. Premature menopause. Ann Med Health Sci Res. 2013;3(1):90–95.
- Martin JA, Hamilton BE, Osterman MJK, Driscoll AK, Drake P. Births: Final data for 2017. National Vital Statistics Reports; vol 67 no 8. Hyattsville, MD: National Center for Health Statistics. 2018.
- Stahlman S, Witkop CT, Clark LL, and Taubman SB. Pregnancies and live births, active component service women, U.S. Armed Forces, 2012–2016. MSMR. 2017;24(11):2–9.
- Service Women Action Network (SWAN). Access to reproductive health care: the experience of military women. https://www.servicewomen.org/wp-content/uploads/2018/12/2018ReproReport_SWAN-2.pdf. Accessed 14 April 2019.
- Centers for Disease Control and Prevention. National Center for Health Statistics. Key Statistics from the National Survey of Family Growth–I Listing. https://www.cdc.gov/nchs/nsfg/key_statistics/i.htm. Accessed 14 April 2019.
- Rooney KL, Domar AD. The relationship between stress and infertility. Dialogues Clin Neurosci. 2018 Mar;20(1):41–47.
- Armed Forces Health Surveillance Center. Health of women after wartime deployments: correlates of risk for selected medical conditions among females after initial and repeat deployments to Afghanistan and Iraq, active component, U.S. Armed Forces. MSMR. 2012;19(7):2–10.
- Van Heertum K, Rossi B. Alcohol and fertility: how much is too much? Fertil Res Pract. 2017;3:10.
- McKee DL, Hu Z, Stahlman S. Incidence and sequelae of acute pelvic inflammatory disease among active component females, U.S. Armed Forces, 1996–2016. MSMR. 2018;25(10):2–8.
- Stahlman S, Oetting AA. Mental health disorders and mental health problems, active component, U.S. Armed Forces, 2007–2016. MSMR. 2018;25(3):2–11.
- Stahlman S, Witkop CT, Clark LL, and Taubman SB. Contraception among active component service women, U.S. Armed Forces, 2012–2016. MSMR. 2017;24(11):10–21.
- Armed Forces Health Surveillance Branch. Absolute and relative morbidity burdens attributable to various illnesses and injuries, active component, U.S. Armed Forces, 2018. MSMR. 2019;26(5):2–9.
- Armed Forces Health Surveillance Branch. Ambulatory visits, active component, U.S. Armed Forces, 2018. MSMR. 2019;26(5):18–24.
- Armed Forces Health Surveillance Center. Female infertility, active component service women, U.S. Armed Forces, 2000–2012. MSMR. 2013;20(9):8–12.
- Jose-Miller AB, Boyden JW, Frey KA. Infertility. Am Fam Physician. 2007;75(6):849–56.
- TRICARE. Assisted Reproductive Services. https://www.tricare.mil/CoveredServices/IsItCovered/AssistedReproductiveServices. Accessed 30 April 2019.
- Stahlman S, Seliga N, Oetting AA. Sexually transmitted infections, active component, U.S. Armed Forces, 2010–2018. MSMR. 2019;26(3):2–10.
- Armed Forces Health Surveillance Center. Uterine fibroids, active component females, U.S. Armed Forces, 2001–2010. MSMR. 2011;18(12):10–3.
- Centers for Disease Control and Prevention. National Institute for Occupational Safety and Health. Aircrew Safety and Health: Reproductive Health. https://www.cdc.gov/niosh/topics/aircrew/reproductivehealth.html. Accessed 30 April 2019.