What Are the New Findings?
Between 11 March 2020 and 30 Sept. 2020, a total of 225 ADSMs with a COVID-19 diagnosis had been air evacuated in CENTCOM and EUCOM Areas of Responsibility. The largest demographic proportion of AEs were among service members aged 30-39 years, males, and Army members.
What Is the Impact on Readiness and Force Health Protection?
COVID-19 infections necessitate rigorous adherence to isolation measures to protect the health of the uninfected members of the force. Such measures can severely reduce the availability of many service members for duty. Protective measures such as wearing a mask, washing hands, and social distancing should continue to be taken to prevent continued COVID-19 transmission in theater.
Abstract
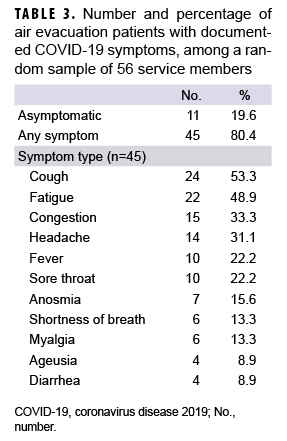
This report documents the numbers of air evacuations for diagnoses of coronavirus disease 2019 (COVID-19) among U.S. active duty service members (ADSMs) from locations in U.S. Central Command (CENTCOM) and U.S. European Command (EUCOM) areas of responsibility. Counted were COVID-19 evacuations both within and out of each of the theaters from 11 March through 30 September 2020. Of the 186 evacuations originating in CENTCOM, 185 resulted in the patients arriving at Landstuhl in EUCOM and 1 was within theater. A total of 169 of the CENTCOM evacuations took place in June through Aug. 2020 and only 1 occurred in Sept. Of the 39 air evacuations originating in EUCOM, 38 were intra-theater transfers and 1 was to a CONUS facility. Most (n=32) of the EUCOM evacuations occurred in Sept. Evacuees were most often members of the Army (71%), enlisted personnel (63%), males (91%), and aged 30 years or older (58%). Among a random sample of 56 evacuees, 20% were asymptomatic. Among those with symptoms, the most common were cough, fatigue, congestion, headache, and sore throat.
Background
The ongoing pandemic of coronavirus disease 2019 (COVID-19) has been caused by the transmission of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which was first identified in Dec. 2019 in Wuhan, China. The World Health Organization (WHO) declared a Public Health Emergency of International Concern in Jan. 2020, and a pandemic in March 2020. As of 10 Dec. 2020, more than 69 million cases have been confirmed, with more than 1.5 million deaths attributed to COVID-19 worldwide.1,2
As in the civilian sector, the COVID-19 pandemic has had a large impact on the Military Health System (MHS), both in the continental U.S. (CONUS) and outside the continental U.S. (OCONUS). As of 10 Dec. 2020, a cumulative total of 108,838 cases of COVID-19 have been reported among MHS beneficiaries, including 72,671 in active duty service members (ADSMs). Roughly 9% of these cases occurred in OCONUS locations. Also, as of 10 Dec., a total of 492 cases of COVID-19 were reported among ADSMs in 7 countries in the U.S. Central Command (CENTCOM) area of responsibility (AOR): 171 in Kuwait, 79 in Afghanistan, 95 in Iraq, 89 in Afghanistan, 41 in the Kingdom of Saudi Arabia, 48 in Qatar, 29 in UAE, and 29 in Bahrain. In the U.S. European Command (EUCOM) AOR, there were 2,443 cases of COVID-19 reported in ADSMs: 1,769 in Germany, 317 in Italy, 165 in the UK, 76 in Spain, 48 in Turkey, 44 in Belgium, and 4 in Romania.2
Management of service members deployed to OCONUS locations who are affected by COVID-19 constitutes a challenging task. During the pandemic, additional considerations must be incorporated into the existing medical management action plans and new guidance implemented. According to the U.S. CENTCOM COVID-19 Pandemic Playbook for Operational Environment guidance, all persons who test positive for COVID-19 need to be moved into isolation and prepared for evacuation to OCONUS or CONUS locations as designated by the evacuation plan in that region. However, this playbook was intended to be used as guidance rather than a standard of care.3
In 2014, during Operation United Assistance in support of the Ebola outbreak, U.S. Africa Command (AFRICOM) identified the need to move patients exposed to High Consequence Infectious Disease out of the African theater of operations to the continental U.S. This requirement was tasked to U.S. Transportation Command (TRANSCOM), which then created a Joint Urgent Operational Needs Statement. The Air Mobility Command aircrew and medical personnel also created the Transport Isolation System (TIS) to fulfill this task.4 The TIS is an infectious disease containment unit designed to minimize contamination risk to aircrew, medical attendants, and the airframe while allowing medical care to be provided to patients in-flight.4 On 10 April 2020, the first use of TIS for the movement of COVID-19 positive patients (3 contractors) was conducted aboard U.S. Air Force aircraft, from Afghanistan to Ramstein Air Base in Germany.5
The objective of this study was to perform a descriptive analysis of air evacuations for COVID-19 executed in the CENTCOM and EUCOM AORs from 11 March 2020 through 30 Sept. 2020.
Methods
Air evacuations for COVID-19 infected patients were identified using data from the U.S. Transportation Command (TRANSCOM) Regulating and Command & Control Evacuation System (TRAC2ES). TRAC2ES combines transportation, logistics, and clinical decision elements into an automated patient movement information system. The surveillance population included all ADSMs who were air evacuated from CENTCOM and EUCOM with a COVID-19 diagnosis (International Classification of Diseases, 10th Revision [ICD-10] code: U07.1) in any of the 3 diagnostic positions (DX1-DX3). These air evacuations included evacuations both within the same theater and evacuations out of theater into another AOR. The surveillance period was from 11 March 2020 through 30 Sept. 2020. Microsoft Excel 2013 (Microsoft Corporation, Redmond, WA) was used to conduct a descriptive analysis, including numbers and percentages of evacuations by location, time, military branch, rank, age group, and sex. Using the Mersenne Twister Algorithm in Excel, a random sample representing 25 percent of the study population (n=56) was selected to characterize symptoms of COVID-19 reported in the TRAC2ES air evacuation record.
Results
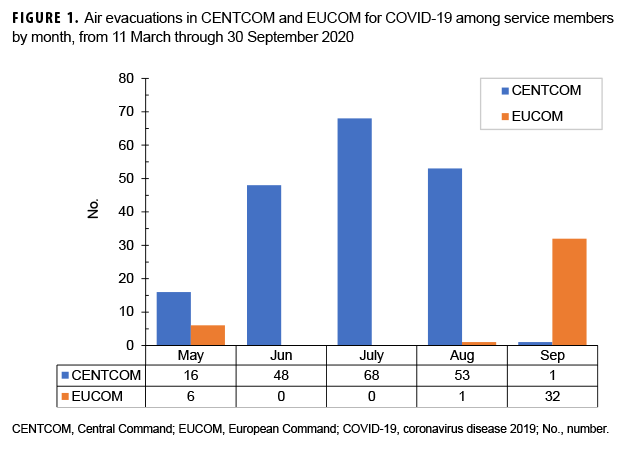
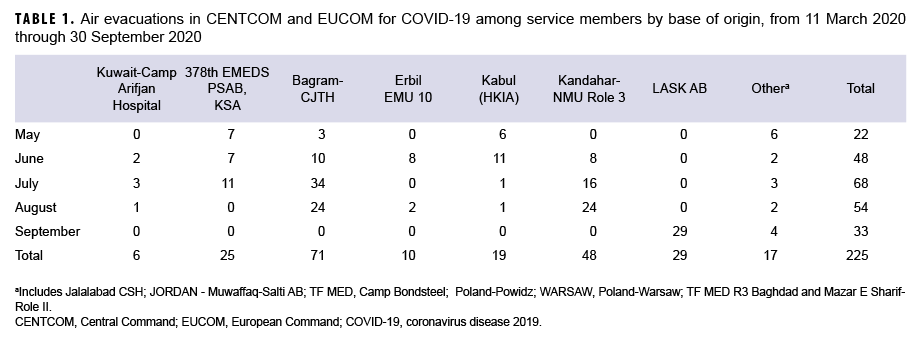
By the end of September 2020, 225 ADSMs with a COVID-19 diagnosis in TRAC2ES had been air evacuated in CENTOM or EUCOM. Of all air evacuations (AEs), 83% (n=186) originated in CENTCOM, whereas 17% (n=39) originated in the EUCOM (Figure 1). Of the air evacuations originating in CENTCOM, 185 of these were evacuated to Landstuhl in EUCOM, and 1 was evacuated to Craig Joint Theater Hospital in Bagram. Of the air evacuations originating in EUCOM, 38 of these were intra-theater transfers (31 to Spangdahlem Air Base, 7 to Landstuhl), and 1 was to a CONUS facility. The bases of origin with the largest number of AEs were: Craig Joint Theater Hospital, Bagram Airfield (n=71) and Multinational Medical Unit, Kandahar Airfield (n=48) in Afghanistan (CENTCOM), followed by Lask Air Base (n=29) in Poland (EUCOM) (Table 1, Figure 2).
The number of AEs were relatively constant during the months of June, July, Aug. (n=48, n=68, n=53 respectively) in the CENTCOM AOR. Conversely, in EUCOM, after an initial low tally during the first 4 months of May, June, July and Aug., a peak was reached in September with 32 AEs. Overall, the highest number of AEs executed in a given month was seen in July with 68 completed AEs (Figure 1).
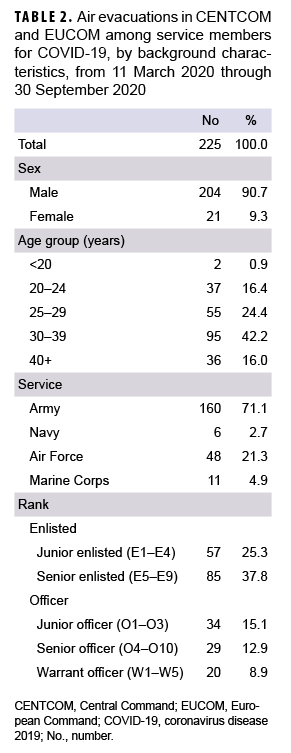
Across service branches, the Army had the highest number of COVID-19 diagnosed patients being air evacuated (n=160), which represented 71% of total AEs, followed by the Air Force with 21% (n=48), and the Navy and Marine Corps with 8% combined (n=17) (Table 2). Among ranks, a higher number of AEs was noted among enlisted personnel, with 63% (n=142) of AEs occurring among enlisted personnel compared to Officers, including Warrant Officers, who constituted 37% (n=83). Patients aged 30 to 39 years made up almost half of those who were air evacuated (42%, n=95). Males accounted for 91% (n= 204) of all AEs. (Table 2).
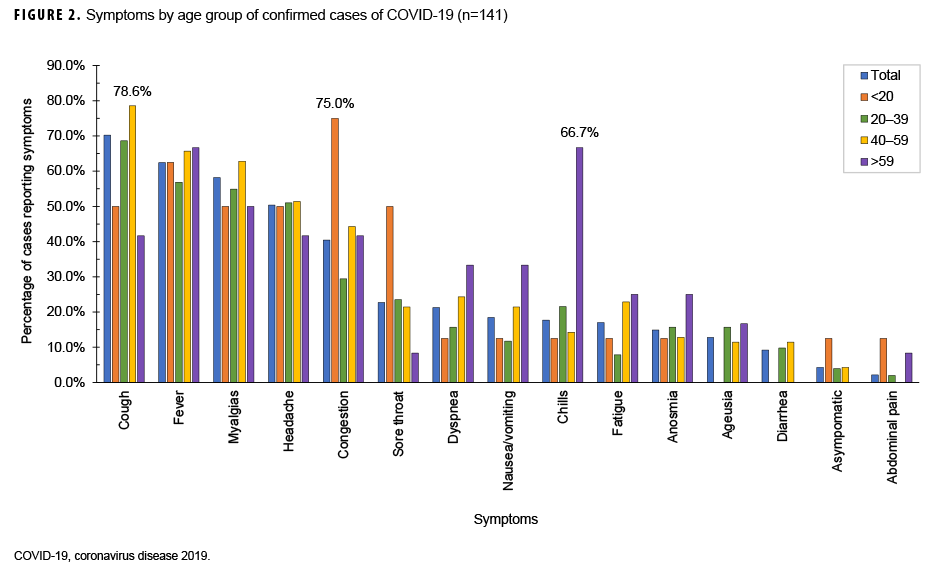
Among the 56 AEs randomly selected from the study population, 20 percent (n=11) were asymptomatic and 80 percent (n=45) had documentation of various symptoms including cough (53%, n=24), fatigue (49%, n=22), congestion (33%, n=15), headache (31%, n=14), fever (22%, n=10), sore throat (22%, n=10), anosmia (loss of sense of smell) (16%, n=7), shortness of breath (13%, n=6), myalgia (13%, n=6), ageusia (loss of sense of taste) (9%, n=4) and diarrhea (9%, n=4) (Table 3).
Editorial Comment
This report documents 225 AEs in CENTCOM (n=186) and EUCOM (n=39) AORs of service members with a diagnosis for COVID-19 through the end of Sept. 2020. The majority of AEs occurred among Army personnel, males, enlisted personnel, and those 30 years of age and older. Compared to the population distribution of ADSMs from Jan. 2020, service members who had an AE were disproportionately Army members (72% vs. 35%), male (91% vs. 83%), and aged 30-39 years (42% vs. 28%). To some extent, this reflects the distribution of the deployed population (with the majority being males in the Army). However, the finding that many AEs occurred among relatively older service members (30 years of age or more) could also suggest that older members are more likely to be evacuated potentially because they are more likely to manifest symptoms and subsequently to be tested. The random sample chosen for analysis of symptoms suggested that most patients with an AE had a mild to moderate clinical presentation that was dominated by upper respiratory complaints, predominantly cough, fatigue, congestion, and headache. There were a few cases with gastrointestinal conditions (4 patients with diarrhea).
Most AEs were executed out of Afghanistan (n=119) from Craig Joint Theater Hospital, Bagram Airfield and Multinational Medical Unit (MMU), Kandahar Airfield. This is not surprising given that the 455th Expeditionary Medical Group (EMDG) is the medical component of Task Force Medical-Afghanistan operating at the Craig Joint Theater Hospital at Bagram Airfield Afghanistan. The EMDG provides combat medical services and support to U.S. and coalition forces throughout Afghanistan. Additionally, it serves as a hub for all aeromedical evacuation missions within the Combined Joint Operations Area-Afghanistan. From here, U.S. and Coalition members are flown to Landstuhl or the United States within 24–72 hours by aeromedical evacuation or a critical care air transportation team.
In 2019, there were 1,142 AEs among service members out of CENTCOM.6 Of these, only 4 (0.4%) were attributed to infectious and parasitic diseases (ICD-10: L00–B99) and 16 (1.4%) were attributed to respiratory system conditions. This indicates that the number of AEs for COVID-19 in 2020 was ten times higher than that for infectious disease and respiratory system conditions in 2019. However, it should be taken in consideration that COVID-19 is unique in nature because, as specified in the COVID-19 Pandemic Playbook for Operational Environment guidance, all persons who test positive for COVID-19 needed to be moved into isolation and prepared for evacuation to OCONUS or CONUS locations. This would not have been the case in previous years for other respiratory or infectious diseases, and as such, this policy is likely one explanation for the high number of service members air evacuated out of theater for COVID-19. In addition, it is important to note that many of the air evacuations described in this report were not medically indicated. For example, several of the evacuations from Lask Air Base to Spangdahlem were noted as being close contacts of positive cases. Despite this, the high number of AEs for COVID-19 to date suggest that COVID-19 has had and will likely continue to have an impact on in-theater military operations.
A limitation of this study is the lack of denominator data including the deployed population of service members during the surveillance period, which resulted in the inability to calculate rates of AEs. This makes it more difficult to determine whether the members of demographic and military groups listed above were over or underrepresented among the evacuees. In addition, misclassification of the outcome (COVID-19 infection) is possible and in particular for those who were evacuated on the basis of being a close contact, because not all of these may have been true cases of COVID-19. However, most of the evacuation records reported that the patient was positive via laboratory test.
Overall, this study indicates the need for flexibility and adaptability of the health force in accordance with unpredicted environmental rigors. There will likely be continued difficulty in finding cost-effective solutions for managing COVID-19 patients in theater, given the rapidly changing dynamic of the pandemic. However, additional analyses are needed to evaluate the effectiveness of current force health protection policies such as Restriction of Movement (ROM), a general DOD term referring to quarantine and isolation for the purpose of ensuring health and safety to prevent continued COVID-19 transmission in theater, as well as enforcing basic protective measures such as wearing a mask, practice of hand hygiene, and social distancing.
Author affiliations: Uniformed Services University of Health Sciences, Bethesda, MD (LCDR Stanila); Amed Forces Health Surveillance Division (CAPT Wells, Drs. Stahlman and Ziadeh).
References
- Johns Hopkins University. Coronavirus Resource Center. https://coronavirus.jhu.edu/. Accessed 11 Dec. 2020.
- Armed Forces Health Surveillance Division. AFHSD Global COVID-19 Surveillance Summary #47, 10 Dec. 2020. https://health.mil/Military-Health-Topics/Combat-Support/Armed-Forces-Health-Surveillance-Branch/Integrated-Biosurveillance/Health-Surveillance-Explorer. Accessed 10 Dec. 2020.
- U.S. CENTRAL COMMAND. 12 May 2020. U.S. CENTRAL COMMAND COVID-19 PANDEMIC PLAYBOOK FOR OPERATIONAL ENVIRONMENTS. https://jts.amedd.army.mil/assets/docs/USCENTCOM_COVID-19_Pandemic_Playbook. pdf. Accessed 11 Dec. 2020.
- Air Mobility Command. Transport Isolation System (TIS). 1 April 2020. https://www.amc.af.mil/About-Us/Fact-Sheets/Display/Article/2132917/transport-isolation-system-tis/. Accessed 10 Dec. 2020.
- Pawlyk, Oriana. Air Force Uses Cutting-Edge Isolation Pod to Evacuate COVID-19 Patients from Afghanistan. https://www.military.com/dailynews/2020/04/14/air-force-uses-cutting-edgeisolation-pod-evacuate-covid-19-patients-afghanistan. html. Accessed 14 Dec. 2020.
- Armed Forces Health Surveillance Division. Medical evacuations out of the U.S. Central Command, active and reserve components, U.S. Armed Forces, 2019. MSMR. 2020;27(5):27–32.