Defense Health Agency Director: Vaccine rollout safe and effective
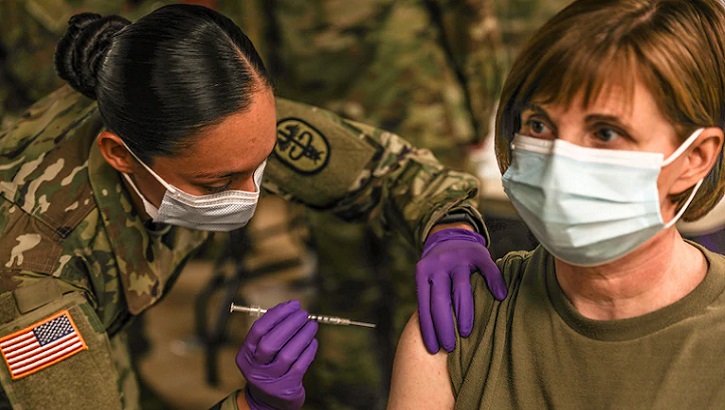 Army Staff Sgt. Brenda Collins administers the COVID-19 vaccine to a patient after its arrival at Fort Hood, Texas, Dec. 15, 2020. (Photo by Army Staff Sgt. Desmond Cassell.)
Army Staff Sgt. Brenda Collins administers the COVID-19 vaccine to a patient after its arrival at Fort Hood, Texas, Dec. 15, 2020. (Photo by Army Staff Sgt. Desmond Cassell.)
The Department of Defense (DOD) moved quickly to ensure a safe and effective rollout of the first COVID-19 vaccine, and began inoculating front line healthcare workers and first responders since initial allocations of the vaccine were delivered beginning Dec. 14, according to Defense Health Agency Director Lt. Gen. (Dr.) Ronald Place.
“Thirteen military communities in the United States received their vaccine doses on time and within 24 hours of receipt, we began administering the vaccine according to plan,” Place said.
Immediately after the Food and Drug Administration issued an emergency use authorization for the Pfizer-BioNTech vaccine Dec. 12, DOD mobilized to distribute approximately 44,000 initial doses to those first 13 communities. This was the first step of a phased and coordinated plan developed over months to prioritize, distribute, and ultimately begin to vaccinate DOD personnel.
“As the vaccine becomes more widely available in the coming weeks, we strongly encourage everyone to get vaccinated,” Place stressed. “The vaccine is safe, effective, and a critical addition to current public health measures. It helps us protect our health, our families, our communities, and significantly decrease the public health risks associated with the COVID-19 pandemic.”
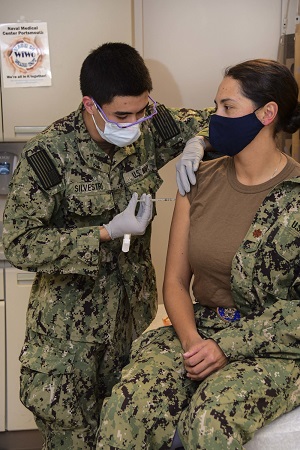 Navy Hospitalman Roman Silvestri administers one of the first COVID-19 vaccines given at Naval Medical Center Portsmouth (NMCP) to Navy Lt. Cmdr. Daphne Morrisonponce, an emergency medicine physician, Dec. 15. (Photo by Navy Seaman Imani Daniels, Naval Medical Center Portsmouth.)
Navy Hospitalman Roman Silvestri administers one of the first COVID-19 vaccines given at Naval Medical Center Portsmouth (NMCP) to Navy Lt. Cmdr. Daphne Morrisonponce, an emergency medicine physician, Dec. 15. (Photo by Navy Seaman Imani Daniels, Naval Medical Center Portsmouth.)
Place said the DHA is gathering real-time data from the pilot sites to fine-tune any process issues in advance of larger scale distribution. “We are intensely focused on the feedback we are getting because these initial sites form the foundation to validate our distribution, administration, and reporting processes, which will then inform how we expand to additional distribution sites,” he said.
Place added, “It’s also important to recognize the Operation Warp Speed team and our colleagues at the Defense Logistics Agency for their exceptional work over the past week in delivering the vaccine to our medical treatment facilities.”
First shots in arms
Within hours of receiving the shipments, prioritized DoD personnel at each location were in line to receive the vaccine, moving toward “the beginning of the end of the COVID pandemic,” according to Army Col. Martin Doperak, commander of Tripler Army Medical Center in Honolulu, Hawaii.
Until vaccines can be allocated to all of DOD’s 11.1 million personnel, critical medical staff and first responders on the front lines of the COVID fight at each medical facility are first in line.
At Wilford Hall Ambulatory Surgical Center aboard Joint Base San Antonio-Lackland, Texas, Air Force Maj. Andrew Gausepohl, medical director of the 59th Air Wing’s Family Emergency Center, was first in the San Antonio military health system to receive the vaccine Dec. 14.
“It was clearly an honor to be the first in line,” he said. “It wasn’t for me. It was for my patients.” Wilford Hall is part of the San Antonio Medical Health System, the largest among the armed services.
Navy Medical Center San Diego also received its initial shipment Dec. 14 and started vaccinating the following day to healthcare workers within the emergency department and intensive care unit as well as local installation emergency medical services, fire, and police departments from six local Navy and Marine Corps installations it serves.
 Air Force Airman 1st Class Kimber Bernau, 59th Medical Wing Family Emergency Clinic medical technician, administers the Pfizer COVID-19 vaccine shot to Air Force Tech Sgt. Jason Bailey, Dec. 14, 2020, at Wilford Hall Ambulatory Surgical Center, Joint Base San Antonio-Lackland, Texas. The Department of Defense is implementing a standardized and coordinated strategy for prioritizing, distributing, and administering the COVID-19 vaccine through a phased approach to all Active Duty, Reserve, National Guard, and all mission-essential DOD civilian employees and other personnel. (Photo by Air Force Airman 1st Class Melody Bordeaux.)
Air Force Airman 1st Class Kimber Bernau, 59th Medical Wing Family Emergency Clinic medical technician, administers the Pfizer COVID-19 vaccine shot to Air Force Tech Sgt. Jason Bailey, Dec. 14, 2020, at Wilford Hall Ambulatory Surgical Center, Joint Base San Antonio-Lackland, Texas. The Department of Defense is implementing a standardized and coordinated strategy for prioritizing, distributing, and administering the COVID-19 vaccine through a phased approach to all Active Duty, Reserve, National Guard, and all mission-essential DOD civilian employees and other personnel. (Photo by Air Force Airman 1st Class Melody Bordeaux.)
“I’m grateful that we have the opportunity to participate in such a historic public health event that will have a profound impact on the health of our staff and the Department of Defense family we serve,” said Navy Cmdr. Jason Rice, NMCSD’s director of public health and public health emergency officer.
The next day, Navy Medical Center Portsmouth, Virginia, received its initial allocation. “We are honored to be selected as one of the first military treatment facilities to receive the COVID-19 vaccine,” said Navy Capt. Lisa Mulligan, commanding officer of NMCP, upon receiving their shipment Dec. 15. The medical center is the Navy’s oldest continuously operating military hospital, serving past and present military members and their families since 1830.
Within two to three days of vaccinating the prioritized group of recipients, NMCSD plans to use the rest of its initial allotment to vaccinate inpatient health care workers and their outpatient counterparts.
Walter Reed National Military Medical Center in Bethesda, Maryland, started vaccinating select medical staff promptly after receiving its initial shipment of vaccines Dec. 14. Acting Secretary of Defense Christopher Miller was present to witness the event and receive his vaccine.
“This is a very important day, not just for the Department of Defense, but for our nation,” he said.
“Our service members, DOD civilians, and their families have demonstrated remarkable endurance and sacrifice throughout the pandemic,” he said before witnessing the first shots. “We know that our collective sacrifice would accelerate the path to a cure and save lives.”
Visit https://www.defense.gov/Explore/Spotlight/Coronavirus/Operation-Warp-Speed/ and www.health.mil/coronavirus to read more about the DoD’s response to the pandemic and ongoing administration of the COVID-19 vaccine.