MHS Transformation results continue during COVID-19
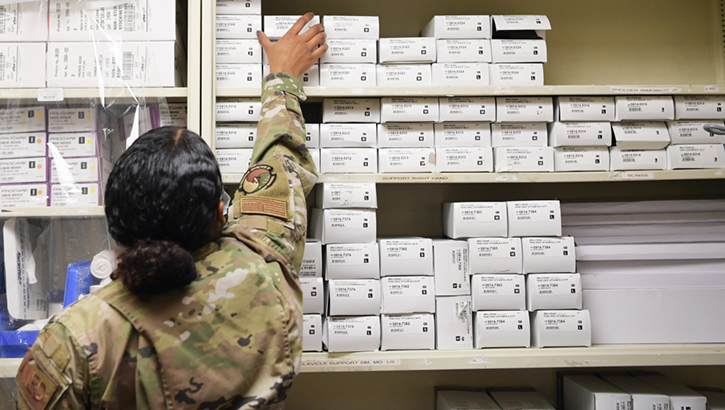 Air Force Staff Sgt. Anjelica Scott, 51st Medical Group medical technician, retrieves supplies at Osan Air Base in the Republic of Korea. Improvements in logistics will continued to improve the way the Military Health System delivers quality care. (Photo by Air Force Senior Airman Noah Sudolcan, 51st Fighter Wing, Osan AB, Repulic of Korea.)
Air Force Staff Sgt. Anjelica Scott, 51st Medical Group medical technician, retrieves supplies at Osan Air Base in the Republic of Korea. Improvements in logistics will continued to improve the way the Military Health System delivers quality care. (Photo by Air Force Senior Airman Noah Sudolcan, 51st Fighter Wing, Osan AB, Repulic of Korea.)
Focusing on that patient-centered approach to care and improving quality of life, is how Dr. Barclay Butler, the Defense Health Agency’s assistant director for management, describes the reason behind the Military Health System’s transformation.
Since October 2018, the Department of Defense began the congressionally directed multi-year transition of military medical treatment facilities from the Services to the DHA. And at the beginning of 2020, the DHA established and successfully transitioned the first wave of hospitals and clinics under its authority, direction, and control (ADC).
Although MTF transition efforts were paused this past April so the Services and DHA could support the national response to the COVID-19 pandemic, the transition was formally restarted this past November. In coordination with the Services, the DHA will continue to transition ADC of all hospitals and clinics to the DHA through September 2021.
 Navy Hospital Corpsman 2nd Class Robert Newkirt, a radiologic technologist assigned to Naval Medical Center San Diego's (NMCSD) Radiology Department, prepares an operating room for an interventional radiology (IR) procedure. (Photo by Navy Seaman Luke Cunningham, Naval Medical Center San Diego.)
Navy Hospital Corpsman 2nd Class Robert Newkirt, a radiologic technologist assigned to Naval Medical Center San Diego's (NMCSD) Radiology Department, prepares an operating room for an interventional radiology (IR) procedure. (Photo by Navy Seaman Luke Cunningham, Naval Medical Center San Diego.)
This transition has enabled the DHA to increase standardization, eliminate duplicative contracts, and realize cost efficiencies by beginning the management of an enterprise-wide program to fulfill health care requirements in all military medical treatment facilities (MTFs).
“It’s about putting the patient at the center of everything we do,” explained Butler. The DHA has recently taken efforts to quantify its achievements across approximately 30 different functions and documented hundreds of contributions to the MHS.
Some DHA achievements include:
- Yielded $15M of initial savings in the National Capital Region for contracted Medical Q-coded Services by demonstrating a Market-Based Buying Strategy (MBBS) to actively manage demand for products and services in a given market.
- The MHS’s inTransition program, a program that assists service members and veterans who want to get connected to mental health care, conducted mandated outreach calls to approximately 8,500 Service members in October 2020, with 600 of these engaging with the program for formal transition coaching.
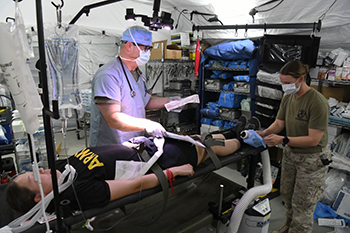 Joint Force medical service members participated in a mass casualty exercise held by 378th Expeditionary Medical Squadron in Nov. at Prince Sultan Air Base, Kingdom of Saudi Arabia. The exercise gave soldiers, Marines and airmen the chance to hone their triage, treatment and medical transportation skills for a large number of simulated wounded in a stressful environment. Improvements to Medical Modeling and Simulation has saved nearly $5 billion since fiscal year 2014. (Photo by Air Force Tech Sgt. Wes Wright, 378th Air Expeditionary Wing.)
Joint Force medical service members participated in a mass casualty exercise held by 378th Expeditionary Medical Squadron in Nov. at Prince Sultan Air Base, Kingdom of Saudi Arabia. The exercise gave soldiers, Marines and airmen the chance to hone their triage, treatment and medical transportation skills for a large number of simulated wounded in a stressful environment. Improvements to Medical Modeling and Simulation has saved nearly $5 billion since fiscal year 2014. (Photo by Air Force Tech Sgt. Wes Wright, 378th Air Expeditionary Wing.)
- Psychological Health Center of Excellence (PHCoE) began a study of antidepressant use and risk for suicide-related outcomes among Active-Duty Service members. The study will provide valuable insight into the association between antidepressant use and suicide risk among Service members. Conclusions drawn from the study could be used to develop new clinical procedures for suicide risk care that may address a heretofore unidentified source of risk.
- The new MTF Annual Regulatory Training saved the MHS 68,713 staff-hours in year one, and 451,491 staff-hours of training time over the next three years. The new training program saves the average MTF trainee 50 minutes the first year and then 2 ½ hours in each of the following two years. This time savings year over year equates to approximately a 40% savings in training time for the regulatory training. For clinicians and specialists, these regulatory training requirements will decrease from 3 ½ hours a year to under 2 hours, increasing their availability to see patients. Similarly, this is a training time savings of45% for this regulatory training. This saving equates to an estimated staff-hour savings of 7,328 staff-hours in year one and 48,907 staff-hours in years two and three.
- The Defense Medical Modeling & Simulation Office (DMMSO) has improved communication and collaboration (breaking down silos) between the Service-specific Medical Modeling and Simulation (MM&S) programs, leading to a total cost savings/avoidance of $4.81 million since its inception in fiscal year 2014.
- Through a new Life Support training conversion, DHA’s new training methodology reduces time away from patient care for both students and instructors by cutting training time for Life Support training by up to 50%, with an estimated time savings of 242,000 staff-hours for students and an additional 12,000 staff-hours for instructors.
- Launched nine enterprise-wide initiatives stemming from the Quadruple Aim Performance Process (QPP) and has documented the demand, supply, and gaps for 123 MTFs and 7 markets. These achievements are part of the DHA’s long-term effort to synchronize the Services and the DHA onto a single, cyclical strategy planning and execution cycle. MTFs from all the Services are now aligning their Strategic Performance Plans to a single (DHA) Director’s Guidance as opposed to three separate sets of guidance from each of the Services.446 Strategic Initiatives were submitted in alignment with DHA Guidance during FY20.
- A recent Defense and Veterans Brain Injury Center (now Traumatic Brain Injury Center of Excellence) study may aid in returning the warfighter to duty status quicker, as well as create a pathway to new treatment interventions for service members.
MHS transformation efforts were driven by Section 702 of the Fiscal Year 2017 National Defense Authorization Act and subsequent guidance provided by Congress in 2018, 2019, and 2020 that directed the MHS reorganization, redefining the roles of the military medical departments and the DHA in the administration and management of hospitals and clinics.
As the single agency in charge of all MTFs, the DHA will create a more integrated, efficient, and effective system of medical readiness and health care delivery. “Throughout our response to the COVID-19 pandemic and the MTF transition efforts, the DHA continues to focus on ensuring the continuation of the Department of Defense’s top three priorities— protect the DOD’s people, maintain military readiness, and support the whole-of-government interagency response,” concluded Butler.
For more information on the Military Health System Transformation, visit the MHS Transformation.