What are the New Findings?
Influenza remains a threat during military exercises even in highly immunized populations mainly because of the virus's ability to cause illness in large numbers of soldiers which can overload an austere medical system designed mainly to care for traumatic injuries. Use of low-intensity clinical isolation areas is one means of limiting influenza's impact on major exercises scheduled during expected influenza transmission seasons.
What is the Impact on Readiness and Force Health Protection?
Immunization remains the primary force health protection measure for military exercises, but exercises that extend into the Southern Hemisphere may result in the inability to use the most appropriate hemispheric vaccine because of restricted access to products not manufactured for the domestic U.S. market.
Abstract
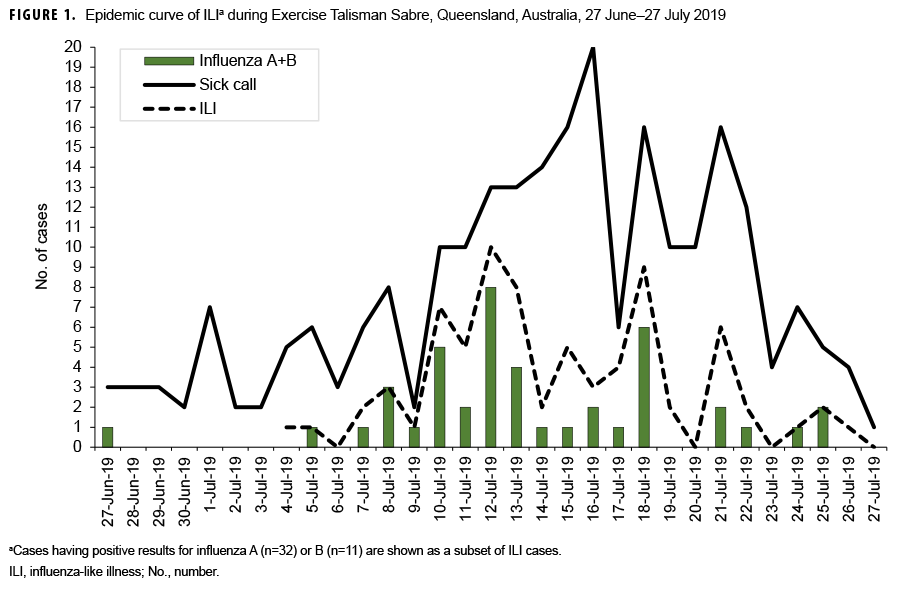
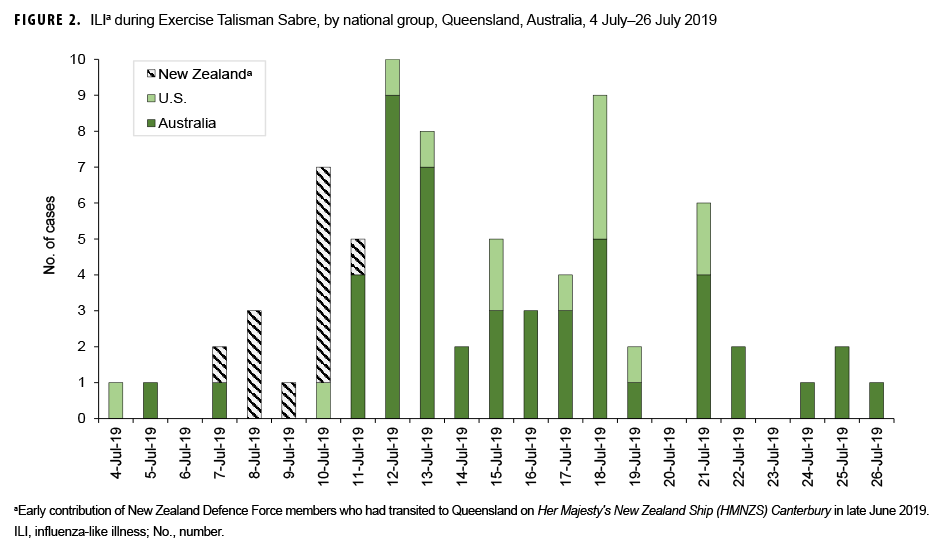
Influenza appeared in Queensland, Australia during Exercise Talisman Sabre (TS-19) in July 2019 with an early focus within the New Zealand Defence Force members arriving in Australia aboard HMNZS Canterbury. A total of 76 cases of influenza-like illness (ILI) were reported, of which 43 were confirmed by rapid diagnostic tests to be influenza A (n=32) and B (n=11). Australia’s influenza season (starting in March, peaked in July 2019) exposed large numbers of military members to a virus for which they had been suboptimally immunized either because of low uptake of the Southern Hemisphere vaccine by Australians/New Zealanders who were not mandated to be immunized, or because U.S. soldiers had received only the Northern Hemisphere vaccine for the 2018–2019 season. A low-intensity clinical unit separate from the main exercise was used as a means of isolating ILI cases both to facilitate their treatment and limit disease spread. Despite disease rates of <1%, influenza still had a major impact on TS-19 mostly in terms of the considerable medical resources required to manage ILI.
Background
Joint and combined military exercises concentrate large numbers of military members under circumstances that favor introduction of new viruses into stressed populations. Currently, the risk influenza poses to military exercises is not mass mortality but mass casualties that could overwhelm the usually limited medical support capabilities designed mainly to treat traumatic injuries during field exercises. This report summarizes an influenza epidemic that occurred within a combined military exercise, Talisman Sabre (TS-19), which took place in Queensland, Australia during July–August 2019.
Talisman Sabre is a long-running series of military exercises in which more than 32,000 soldiers, sailors, and marines mainly from Australia, New Zealand, and the U.S. gather in Queensland in northeastern Australia at mid-year for a 3-week field exercise. Although each national contingent operates under its own command chain, there is considerable intermixing of forces. Southern Hemisphere influenza transmission season occurs at midyear with a usual peak in August/September.
In 2009, when the influenza A(H1N1) virus's potential was not yet known, advanced diagnostic capability was deployed into the field during Talisman Sabre and enabled the detection of 12 persons with the pandemic influenza strain.1 Fortunately the pathogenic potential of the 2009 influenza A(H1N1) strain was inferior to its distant predecessor of 1918, and there was no serious disruption of the exercise although some naval units were removed from participation when influenza appeared shipboard.
Immunization remains the primary force health protection measure against influenza, although protection may be suboptimal depending on the degree to which the vaccine strains chosen for production match the viruses that eventually circulate. Although U.S. forces have high immunization participation rates because influenza vaccination is mandatory, they are immunized with vaccine tailored for the Northern Hemisphere and have usually been immunized more than 6 months prior to TS-19. While influenza immunization of Australian and New Zealand soldiers is strongly encouraged, it is not mandatory for exercise participation, and immunization rates are usually less than ideal.
Additional concerns regarding influenza during TS-19 were generated by the early start to the influenza season in March 2019 in Australia. The start of this season was dominated by influenza A(H3N2) viruses reminiscent of the relatively severe 2017 season (the so-called "Aussie flu").2 The U.S. Indo-Pacific Command (INDOPACOM) Surgeon's office had investigated the possibility of using the Southern Hemisphere influenza vaccine for U.S. forces during port visits of USS Carl Vinson to Sydney in June 2019, but timing and supply issues made such use of the vaccine impractical.
Methods
As the largest scheduled series of military exercises in Australia, the biennial TS-19 involved a great deal of preliminary healthcare planning which began during planning conferences in Hawaii in October 2018 and March 2019. Influenza was an identified medical threat subject to usual precautions and immunization. Deployed forces were supported by a Role 1 clinic (basic ambulatory care) at Rockhampton, a holding/isolation ward at Williamson Airfield, and a Role 2+ (enhanced care) facility from the 2nd General Health Battalion at Shoalwater Bay, as well as on-board medical capability from USS Wasp, HMAS Canberra, and HMAS Adelaide. Disease surveillance systems were instituted upon buildup to the official start of the exercise on 17 June 2019.
Influenza-like illness (ILI) was defined as an illness marked by fever greater than 100 °F with either cough or sore throat in the absence of a known cause other than influenza. Influenza testing was performed on nasal swabs using a rapid detection test, the Quidel QuickVue Influenza A+B test. All influenza-positive samples were then confirmed via polymerase chain reaction testing on the Biofire FilmArray using the Respiratory Panel 2 plus by the pathology department at the Role 2+ facility.
Results
ILI cases initially appeared among the New Zealand Defence Force (NZDF) contingent, which had arrived largely aboard the HMNZS Canterbury on or about 7 July 2019 after a 3-day transit from Auckland. Investigation of the ship's berthing arrangements indicated person-to-person spread of ILI in up to 12 cases while shipboard. The major concern was that the occurrence of several cases of influenza early in the exercise foreshadowed a much larger problem that would arise later when many more soldiers were involved under austere field conditions. A communicable disease plan was revised and instituted in early July 2019. The emphasis was on rapid identification of ILI cases and patient management in Rockhampton away from the main body of troops, which represented more an isolation effort than a quarantine effort. A 20-bed low-intensity clinical facility was set up (with contingency plans for another 20 beds if required) and largely staffed by Australian Defence Force (ADF) reserve component members. Patients did not require inpatient care but could not be left in an austere field environment with ILI symptoms. Oseltamivir was provided for treatment and to reduce infectiousness among those found to be rapid diagnostic test-positive for the influenza virus.
From 17 June 2019 through 27 July 2019, 254 sick call visits were recorded at the various medical treatment units and 76 patients were diagnosed with ILI on clinical grounds. Of the 76 ILI cases that were identified, 32 (42.1%) tested positive for influenza A and 11 (14.5%) for influenza B. These illnesses represented a substantial proportion of all sick call visits during TS-19 as shown in Figure 1. The remaining 33 tests (43.4%) were negative for influenza virus. National contingent composition is shown in Figure 2 and illustrates the early predominance of cases of influenza among NZDF members aboard Her Majesty's New Zealand Ship (HMNZS) Canterbury. No other shipboard outbreaks were noted. Confirmed influenza cases peaked at 10 per day on 12 July 2019 before the formal start of the exercise (data not shown).
Editorial Comment
Respiratory infections have long been known as threats to military operations and many modern exercises have been disrupted by viruses including influenza.3-4 TS-19 was not unique in this regard, but its location in Australia presented additional challenges. The exercise occurred during the peak of influenza season in the Southern Hemisphere, and the early phase of the outbreak placed particular focus on a naval ship. In addition, there was the possibility that influenza cases would affect a range of national groups (U.S., Australia, New Zealand, Canada, UK, Japan) each employing different approaches to addressing influenza. Rapid diagnostics have evolved to become important tools in the management of ILI; now it is possible to quickly determine whether the causative pathogen is influenza and then manage the public health consequences of a virus with such epidemic potential. For TS-19, a special isolation facility was set up, not because otherwise healthy soldiers were thought to be at risk of life-threatening disease, but rather because of the likelihood that the limited medical capability of usual field medical facilities would otherwise be overwhelmed by sick soldiers. During military exercises in a soldier population which has already been immunized, the remaining option in managing an influenza outbreak consists of isolating ILI cases from uninfected troops who are receiving prophylactic antiviral treatment. Isolation of cases within a health facility away from troops under antiviral treatment is the best way to minimize generalized spread in the population which should have already been immunized. The civilian healthcare system of Queensland was extremely supportive of military medical efforts during TS-19, but it could not be expected to house multiple influenza cases that did not otherwise require hospitalization. The low-intensity clinical facility in Rockhampton was a pragmatic response that worked well to optimize treatment and likely minimized the total number of ILI cases.
Influenza during joint and combined military exercises often is seen as particularly important to Air Forces because responding to the virus may require suspension of flight operations, but naval operations are also vulnerable to influenza. As demonstrated during a 1996 outbreak on the USS Arkansas, even highly vaccinated crews may be subject to high attack rates (42%) which may result in aborted exercises if single individuals with influenza A(H3N2) viruses poorly matched to seasonal influenza vaccine infect the ship's crew.5 The situation was never so dire on HMNZS Canterbury, but it did serve as a focus of initial influenza cases that could have infected a much larger number of soldiers in the absence of an effective communicable disease plan.
Influenza immunization is far from perfect, but there is hope that universal influenza vaccines may eventually be developed that will end the evolutionary arms race conducted each year using seasonal vaccines that are at best modestly effective.6 The particular problem experienced during TS-19 was that the Southern Hemisphere influenza A(H3N2) 2019 vaccine component (A/Switzerland/8060/2017) was an updated version of what the U.S. forces had been immunized against (A/Singapore/INFIMH-16-0019/2016) which used the Northern Hemisphere 2018–2019 vaccine.7 Whether this would have made a difference was unknown, but valid concerns had been raised because during the relatively severe 2017 Australian season the influenza A(H3N2) component's vaccine efficacy was estimated to be 10% (95% confidence interval: -16%–31%).6 Although adequate Southern Hemisphere 2019 vaccine was available, it was not approved by the U.S. Food and Drug Administration as there was no motivation for a manufacturer to register a vaccine not intended for U.S. use. Stringent regulatory authority approval by the Australian Therapeutic Goods Administration existed but was bureaucratically insufficient for use in U.S. forces. Further inquiry regarding exceptions to policy might be useful in improving management of influenza immunization for soldiers outside their usual jurisdiction. Such exceptions may prove important as future influenza pandemics are unlikely to provide sufficient time for preparation of stocks of new vaccines, as was demonstrated during 2009 when vaccine became available only after the peak of the pandemic.
Author Affiliations: Headquarters, Joint Operations Command. Bungendore, NSW, Australia (MAJ van Ash, COL Nasveld); 2nd General Health Battalion, Gallipoli Barracks, Enoggera, QLD, Australia (CAPT Zahra); Australian Defence Force Malaria and Infectious Diseases Institute, Enoggera, QLD, Australia (Dr. Shanks).
Acknowledgements: The authors thank the many military medical personnel from Australia, New Zealand, and the U.S. who helped manage the ill service members during Exercise Talisman Sabre 2019.
Disclaimer: The opinions expressed are those of the authors and do not necessarily reflect those of the Australian Defence Force or the U.S. Department of Defense. Conflicts of interest: The authors do not claim any conflict of interest.
Funding: Authors are employees of the Australian Defence Organization. No specific funding was given for this epidemiological study.
References
1. Inglis TJ, Merritt AJ, Levy A, et al. Deployable laboratory response to influenza pandemic; PCR assay field trials and comparison with reference methods. PloS One. 2011;6(10):e25526.
2. Australian Government Department of Health. Australian Influenza Surveillance Report No. 12– 23 September-6 October 2019. Canberra, Australia: Department of Health; 2019.
3. Shanks GD, Hodge J. The ability of seasonal and pandemic influenza to disrupt military operations. J Mil Veterans Hlth. 2011;19(4):13–18.
4. Sanchez JL, Cooper MJ, Myers CA, et al. Respiratory infections in the US military: recent experience and control. Clin Micro Rev. 2015;28(3):743–800.
5. Earhart KC, Beadle C, Miller LK, et al. Outbreak of influenza in highly vaccinated crew of U.S. Navy ship. Emerg Infect Dis. 2001 May- Jun;7(3):463–465.
6. Coleman R, Eick-Cost A, Hawksworth AW, et al. Department of Defense end-of-season influenza vaccine effectiveness estimates for the 2017–2018 season. MSMR. 2018;25:16–20.
7. CDC. Prevention and control of seasonal influenza with vaccines: recommendations of the advisory committee on immunization practices— United States, 2018–19 influenza season. MMWR. 2018;67(3):1–20.