METC trains dietician techs to build, support a Medically Ready Force
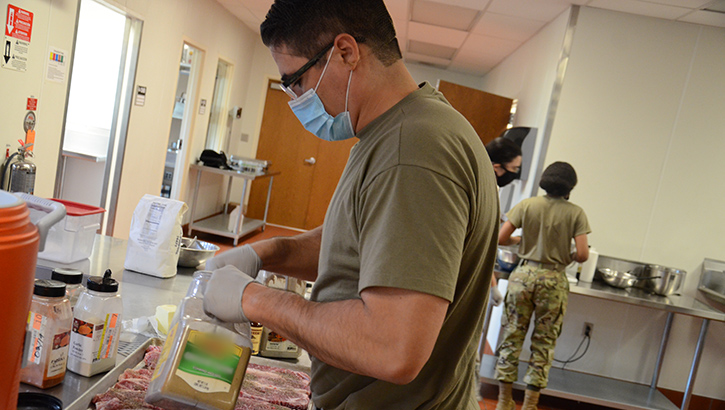 Air Force Master Sgt. Jorge Nikolas, a student in the Nutrition and Diet Therapy program at the Medical Education and Training Campus on Joint Base San Antonio-Fort Sam Houston, Texas, prepares a tray of steaks in the kitchen training laboratory.
Air Force Master Sgt. Jorge Nikolas, a student in the Nutrition and Diet Therapy program at the Medical Education and Training Campus on Joint Base San Antonio-Fort Sam Houston, Texas, prepares a tray of steaks in the kitchen training laboratory.
Good nutrition is the mainstay of health. It is well known that eating the right foods can oftentimes make a big impact on our physical - and mental - wellbeing.
A healthy diet could help fight off illness and control diseases, improve our mood and mental health, and prevent obesity. In fact, the benefits of healthful eating are so well established that medical practitioners employ nutrition therapy to treat certain diseases and chronic conditions.
National Nutrition Month, observed during the month of March, focuses attention on the importance of making informed food choices and developing sound eating habits along with physical activity. Being that health and fitness are synonymous with force readiness, it's no surprise that nutrition plays an important role in the military.
The Nutrition and Diet Therapy program at the Medical Education and Training Campus (METC), located on Joint Base San Antonio-Fort Sam Houston, Texas, trains students to become Army nutrition care specialists or Air Force diet therapy apprentices.
The eight-week long course prepares students to function as entry-level dietetic technicians in medical treatment facilities and deployed settings. Students are taught to perform patient nutrition screenings and assessments, basic medical nutrition therapy, menu and food modification for therapeutic use, how to operate and clean food service equipment, and participate in procurement, storing and administration of dietetic foods and supplies. Students also learn how to prepare an individually-tailored meal based on a nutrition plan designed by a dietician and serve it to a patient.
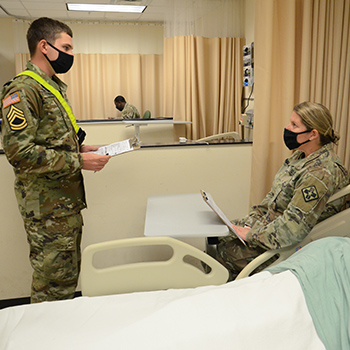 Army Pvt. Tobin Roche, left, conducts a simulated nutrition screening during a practical exercise in the Nutrition and Diet Therapy program at the Medical Education and Training Campus (METC) on Joint Base San Antonio-Fort Sam Houston, Texas. In this portion of the training Roche is learning to conduct nutritional screenings, assessments, and document finding for a simulated patient. Maj. Stephanie Gasper, program director, acts as the patient in this scenario. The METC Nutrition and Diet Therapy program prepares students to function as entry-level dietetic technicians in medical treatment facilities and deployed settings (Photo By: Lisa Braun, Medical Education and Training Campus).
Army Pvt. Tobin Roche, left, conducts a simulated nutrition screening during a practical exercise in the Nutrition and Diet Therapy program at the Medical Education and Training Campus (METC) on Joint Base San Antonio-Fort Sam Houston, Texas. In this portion of the training Roche is learning to conduct nutritional screenings, assessments, and document finding for a simulated patient. Maj. Stephanie Gasper, program director, acts as the patient in this scenario. The METC Nutrition and Diet Therapy program prepares students to function as entry-level dietetic technicians in medical treatment facilities and deployed settings (Photo By: Lisa Braun, Medical Education and Training Campus).
According to Army Maj. Stephanie Gasper, METC Nutrition and Diet Therapy program director, the diversity of the career field covers a wide range of areas that promote and maintain nutrition, health, and readiness within the force.
"Military nutrition technicians can work in food service operations and medical field feeding, sports nutrition to optimize performance and support the warfighter, nutrition for general health and wellness or disease prevention, or perform patient care through medical nutrition therapy for diseases or other conditions in both a hospital and inpatient or ambulatory settings," she explained.
"I think there are so many opportunities for soldiers and airmen in the nutrition career field today compared to several years ago, so I'm excited for what lays ahead of them once they leave here. The majority of our students are excited and ready to take what they learn here to improve the health of our force," Gasper added.
Air Force Master Sgt. Jorge Nikolas, a student in the program, said that Nutrition and Diet Therapy is his dream career field. "The military allowed me to get this training so that I can make a positive impact to the long-term health of my fellow airmen and soldiers. With a large aging population, the country needs more skilled diet therapists to help our currently serving and retired military customers."
The importance of good nutrition cannot be over emphasized.
"Everyone has to eat, and what we eat and how much we eat can have a real impact on our physical and mental wellbeing," Gasper pointed out.