Nurse and Tech Week: Air Force airmen are battle-tested and ready
 Airmen assigned to the 313th Expeditionary Operations Support Squadron transfer a COVID-19 patient following the first-ever operational use of the Negatively Pressurized Conex to transport 12 patients aboard a C-17 Globemaster III aircraft at Ramstein Air Base, Germany last July, to receive higher level of care at the Landstuhl Regional Medical Center, Germany (Photo by: Air Force Airman 1st Class John R. Wright).
Airmen assigned to the 313th Expeditionary Operations Support Squadron transfer a COVID-19 patient following the first-ever operational use of the Negatively Pressurized Conex to transport 12 patients aboard a C-17 Globemaster III aircraft at Ramstein Air Base, Germany last July, to receive higher level of care at the Landstuhl Regional Medical Center, Germany (Photo by: Air Force Airman 1st Class John R. Wright).
This time last year, as the world was trying to wrap its head around an unknown and unforgiving new enemy, Air Force nurses and medical technicians found themselves on the front lines of COVID-19.
Air Force nurses and technicians have remained battle-tested and ready for a fight like this. Saving lives amid insurmountable odds and in the face of unprecedented challenges is what Air Force nurses and technicians remain ready for. The COVID-19 pandemic shined a light on their incredible resilience and dedication to their fellow service members, their patients and their nation.
This week, the Air Force Medical Service recognizes the continued contribution, sacrifice and dedication of its nurses and technicians. These Airmen continue to raise the bar on what it means to serve as an Air Force medic.
A short sample of some of the stories showcasing the work of Air Force nurses and technicians in the past year are highlighted below.
Deployed to nation hotspots
Nurses and technicians deployed to some of the hardest hit areas to provide additional support in overrun hospitals. With short notice, nurses and technicians worked tirelessly alongside sister services and their civilian counterparts to provide critical support when and where the nation needed them.
Air Force Maj. Tynikka Houston, an operating room nurse with the 59th Surgical Squadron, Joint Base San Antonio-Lackland, Texas, deployed in May 2020 as an Individual Mobilization Augmentee assigned to New York Health Hospitals Jacobi. She was assigned to an intensive care unit there to care for COVID-19 patients.
"We basically go wherever they need us," she said.
When the Federal Emergency Management Agency requested additional medical support in North Dakota's hospitals, critical care nurses primarily fulfilled that vital need.
"A short notice CONUS deployment tasking in support of the NORTHCOM combatant commander to fight a pandemic is unprecedented for this medical group," said Air Force Col. Matthew Hanson, 96th Medical Group commander at Eglin Air Force Base in Florida.
"This time, we can't shoot or even see the enemy. We will gown up in our [personal protective equipment] and do our best," said Air Force Capt. Ronald Golemboski, a 96th Health Care Operations Squadron nurse, who had previously deployed to combat zones.
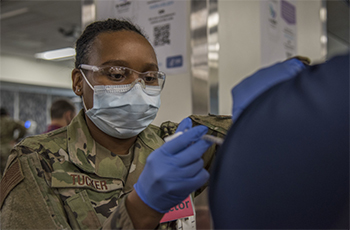 Senior Airman Ladrena Tucker, 59th Medical Operations Squadron Internal Medicine medical technician, administers the COVID-19 vaccine, Feb. 1, 2021, at Wilford Hall Ambulatory Surgical Center, Joint Base San Antonio-Lackland, Texas (Photo by: Air Force Airman 1st Class Melody Bordeaux, 59th Medical Group).
Senior Airman Ladrena Tucker, 59th Medical Operations Squadron Internal Medicine medical technician, administers the COVID-19 vaccine, Feb. 1, 2021, at Wilford Hall Ambulatory Surgical Center, Joint Base San Antonio-Lackland, Texas (Photo by: Air Force Airman 1st Class Melody Bordeaux, 59th Medical Group).
Many Air National Guard and Air Force Reserve medics battled COVID-19 in both their military and civilian roles. Air Force Staff Sgt. Thomas Massa, 192nd Medical Group Detachment 1 aerospace medical technician, has a fulltime job, working as an emergency room medic at Riverside Regional Medical Center in Newport News, Virginia. He also provided COVID-19 response support to the Virginia Department of Emergency Management and the Virginia Department of Health.
"In Detachment 1, we are the people who dress up in hazmat suits and have gas masks on, but one of the things we always practice is putting on our PAPR (Powered Air Purifying Respirator)," Massa said. "The training became useful when COVID started, and we had to intubate more and more people to help them breathe. The medical staff [at Riverside Regional] all had to wear PAPRs. My experience really played a huge part in the COVID response because I could be there to help doctors and nurses put on their PAPRs, something they've never had to do before."
Air Force Capt. Jennifer McGuigan became an Air Force Reserve critical care nurse at age 50 at the height of the pandemic, as the need for additional medical support across the country was critical.
"The need for critical care nurses was highlighted during the response to COVID-19," said Air Force Col. Sherry Hemby, Air Force Reserve Command's command nurse and career field manager. "Many patients diagnosed with COVID-19 had difficulty breathing and were placed on ventilators to assist in their recovery. Critical care nurses, with their amazing attention to detail, were needed to watch every minute. They assessed changes in their patient's condition and reacted with the most skilled care. They pulled patients through the COVID crisis. They held the hands of their patients when their family members could not, encouraging and cheering their patients on to fight for recovery."
Aeromedical Evacuation amid COVID-19
Aeromedical evacuation crews took their capabilities into new territory by transporting COVID-19 patients, ensuring they deliver the same high reliable care seen in the clinic. This is no easy task when it comes to mitigating the spread of a highly infectious respiratory disease in a confined aircraft. Amid the pandemic, nurses and technicians put their experience and training to the test when they flew with the Negatively Pressurized Conex for the first time on July 1, 2020.
"This was definitely not your typical patient movement mission," said Air Force Maj. Benjamin Weaver, bioenvironmental engineer and 10th Expeditionary Aeromedical Evacuation Flight NPC support team lead. "It was a long 22 hours for everyone involved, but the NPC and team performed exceptionally well to make it happen."
Air Force Lt. Col. Penny Cunningham, Pacific Air Forces Command flight nurse, also noted the quick coordination that took place to execute the mission.
"This mission was a great display of how aeromedical evacuation operates, from our logistics team procuring personnel protective equipment kits for pilots and other personnel to ensuring crew bed-down and transportation was firmly established ,"she said. "No matter what AOR we are in, we always have AE members that will support and ensure the mission and crew are taken care of."
Air Force nurses and technicians have a long history of turning aircraft into a flying hospital, treating a wide range of patient challenges and ensuring service members can get to higher levels of care quickly.
 Air Force Tech. Sgt. Steve Zavala, 422nd Medical Squadron medical operations flight chief and trusted care champion, demonstrates COVID-19 testing procedures at RAF Croughton, England last summer (Photo by: Air Force Airman 1st Class Jennifer Zima, 501st Combat Support Wing).
Air Force Tech. Sgt. Steve Zavala, 422nd Medical Squadron medical operations flight chief and trusted care champion, demonstrates COVID-19 testing procedures at RAF Croughton, England last summer (Photo by: Air Force Airman 1st Class Jennifer Zima, 501st Combat Support Wing).
"It's amazing how quickly a non-scheduled mission can spin up and we are sent out the door ready to take on however many patients, any type of health issue from medical health and non-battle injuries to battle injuries," said Maj. Christine Cardoza, 379th Expeditionary Aeromedical Evacuation Squadron flight nurse. "Once in the [aeromedical evacuation] system, the patient's survival rate, I believe, is more than 98%! Being a part of that is an honor in itself."
Innovating to save lives
At both military treatment facilities and civilian hospitals, nurses and technicians had to quickly adapt to COVID-19, developing protocols and procedures to improve lifesaving capabilities and mitigate the spread within the clinic.
For Air Force Maj. Mark Gosling, a registered nurse, 81st Medical Group, Keesler Air Force Base, Mississippi and his Simulation Laboratory Team, this meant modifying the design of their intensive care unit beds to optimize them for ventilated COVID-19 patients.
"The patient is always our number one focus, but this frame of thinking is even more important when you're dealing with critical care from a COVID standpoint," said Gosling. "When you're using ventilator techniques on a patient, they can't tell you what they're feeling, or if they're uncomfortable. They're completely dependent on you and how in tune you are with their needs now and throughout their care. So we need to be thinking multiple steps ahead."
Improving how staff responded to potential COVID-19 symptoms among their patient population fell into the hands of Air Force Airman 1st Class Tara Somers, a medical technician at Landstuhl Regional Medical Center, Germany. She developed an algorithm for staff to use when patients called with possible symptoms, developed a telephone script, and initiated a patient tracker.
"(The process) also provides more complete care to our patients and makes them feel like they are being prioritized when they are feeling afraid in the middle of the pandemic," said Somers. "I am the only technician in the clinic specifically taking on the task. This allows me to follow providers more closely, obtain more knowledge and understanding about the pandemic and the medical threats it presents to our patient population."
Early in the pandemic, medical technicians with the 422nd Medical Squadron at RAF Croughton, England, noticed an issue with testing procedures that relied on seasonal flu procedures. These technicians pushed for clearer guidance to ensure they could obtain more accurate results. Because of medics like Air Force Tech. Sgt. Steve Zavala, 422nd Medical Squadron medical operations flight chief, and his fellow medical technicians, there were necessary improvements in COVID-19 testing procedures implemented across the Department of Defense.
Turning a corner
The rapid production and deployment of COVID-19 vaccines shows a promising shift in the COVID-19 pandemic. Being on the front lines themselves, Air Force nurses and technicians were some of the first to line up to get vaccinated. They also delivered shots in arms to their fellow warfighters ensuring Air Force and Space Force missions continued uninterrupted. Many of these nurses and technicians also supported mass vaccination sites across the country.
"Volunteering to administer the vaccine to patients is important to me because people are dying from this disease," said Air Force Senior Airman Ladrena Tucker, 59th Medical Operations Squadron Internal Medicine medical technician. "I want to help end this pandemic and the least I can do is administer the vaccine."