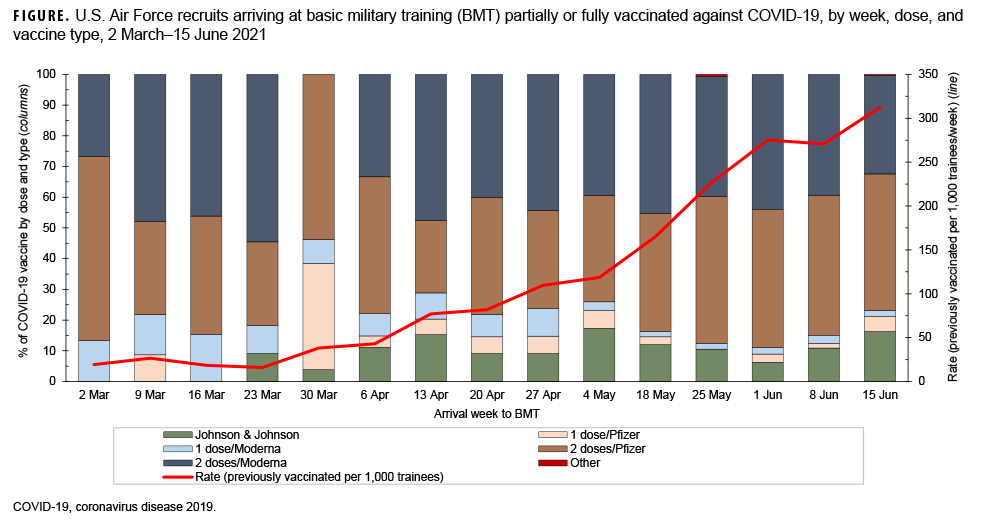
Early in 2021, Air Force basic military trainees began arriving at Lackland Air Force Base either partially or fully vaccinated against coronavirus disease 2019 (COVID-19). During the defined 15-week time frame (March 2–June 15), 600–900 trainees entered basic military training (BMT) on a weekly basis. The rate of trainees who arrived partially or fully vaccinated against COVID-19 per 1,000 trainees increased on a weekly basis in 12 out of the 15 weeks. The lowest rate was 16 previously vaccinated trainees per 1,000 trainees arriving in the week of March 23, 2021 and the peak rate was 313 per 1,000 trainees in the week of June 15, 2021. The Pfizer and Moderna vaccines were the predominant vaccines throughout the period. The majority of trainees who received vaccine against COVID-19 prior to arrival at BMT were fully vaccinated (range: 58%–98% per week).
Author affiliation: Office of the Command Surgeon, Headquarters Air Education and Training Command/SGPJ, Joint Base San Antonio-Randolph, TX (Maj Frankel).
Disclaimer: Material has been reviewed by the 59th Medical Wing Institutional Review Board, and there is no objection to its publication. The opinions or assertions contained herein are the views of the authors and do not necessarily reflect the official policy or position of the U.S. Air Force, the Department of Defense, or the U.S. Government.