Abstract
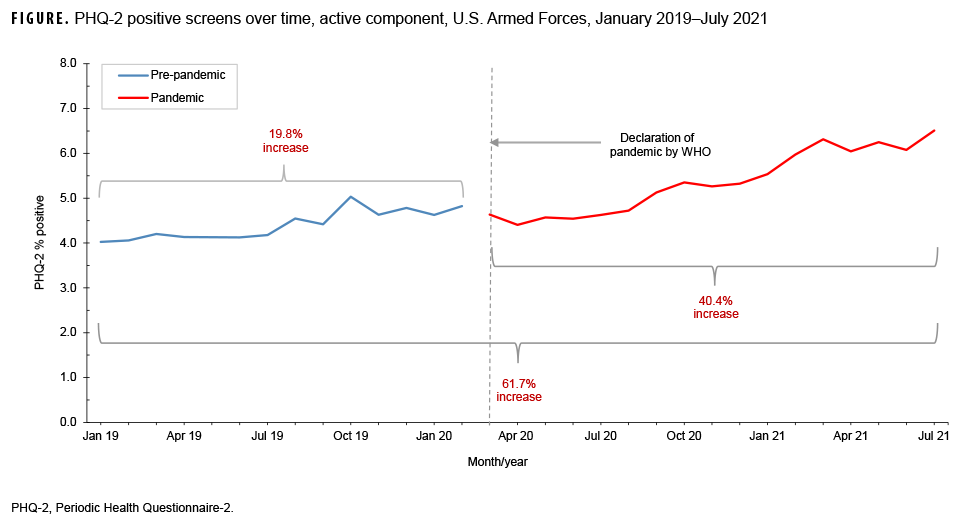
This study examined the rates of depressive symptoms in active component U.S. service members prior to and during the COVID-19 pandemic and evaluated whether SARS-CoV-2 test results (positive or negative) were associated with self-reported depressive symptoms. Depressive symptoms were measured by the Patient Health Questionnaire-2 (PHQ-2) screening instrument and were defined as positive if the total score was 3 or greater. From 1 Jan. 2019 through 31 July 2021, 2,313,825 PHQ-2s were completed with an increase in the positive rate from 4.0% to 6.5% (absolute % difference, +2.5%; relative % change, +67.1%) from the beginning to the end of the period. While there was a gradual increase of 19.8% in the months prior to the pandemic (1.4%/month average), this increase grew to 40.4% during the pandemic (2.5%/month average). However, no association was found between a positive or negative SARS-CoV-2 test result and the PHQ-2 screening instrument result. These findings suggest that the accelerated increase in depressive symptoms is likely a function of the environment of the COVID-19 pandemic instead of the SARS-CoV-2 infection itself. Further research to better understand specific factors of the pandemic leading to depressive symptoms will improve efficient allocation of military medical resources and safeguard military medical readiness.
What Are the New Findings?
The prevalence of depressive symptoms, as measured by a positive result on the PHQ-2 screening instrument, have increased throughout the course of the COVID-19 pandemic. However, SARS-CoV-2 testing status (positive vs. negative) was not associated with reporting of depressive symptoms.
What Is the Impact on Readiness and Force Health Protection?
An improved understanding of the association between depressive symptoms and COVID-19 can inform the targeting of resources to areas of greatest need which would mitigate the degradation of medical readiness of service members.
Background
Worldwide, mental health disorders contribute to 7% of the global burden of disease and 19% of all years lived with disability.1 In the U.S., almost 20% of adults experience a mental health disorder annually.2 One of the most prevalent mental health disorders is depression. Based on results of the 2019 National Health Interview Survey, 18.5% of adults 18 years or older reported experiencing symptoms of depression during the 2 weeks prior to the survey.3 Additionally, the 2019 National Survey on Drug Use and Health estimated that 19.4 million U.S. adults aged 18 or older had at least 1 major depressive episode in the past year (7.8% of all U.S. adults).4 The prevalence of depressive symptoms and major depressive episodes varies by age, sex, and race/ethnicity group with the highest rates among those aged 18–25, women, and non-Hispanic Black and non-Hispanic White adults.5 Likely owing in part to the prerequisite physical and mental fitness standards for accession, the active component U.S. military has experienced lower annual rates of depressive disorders (less than 5% in 2019) than that of the general U.S. population; however, similar to the pattern seen in the civilian population, the rate is higher for female than for male service members (5.1% and 2.4%, respectively).6
First identified in Dec. 2019, COVID-19 was declared a global pandemic by the World Health Organization (WHO) in March 2020.7 As of early Sep. 2021, SARS-CoV-2, the virus that causes COVID-19, has infected over 218 million people and resulted in more than 4.5 million deaths worldwide.8 Within the approximately 1.4 million U.S. active component military members, more than 181,000 individuals have been diagnosed with SARS-CoV-2 infections.9
COVID-19 has affected every facet of society and led to a significant burden on public health practice and medical treatment facilities and has resulted in an upheaval of social norms. While several COVID-19 vaccines now exist, for more than a year, nonpharmaceutical interventions (NPIs) were used to mitigate the spread of SARS-CoV-2. With the emergence of the more contagious Delta variant of SARS-CoV-2, many regions of the country have returned to an increased use of NPIs. The most commonly advocated NPI is social distancing which involves avoiding close contact with any individual who does not live in a person's household.10 Though this practice has been shown to diminish the spread of SARS-CoV-2,11 it also significantly decreases the frequency and diversity of human interaction. Additionally, stressors such as isolation, loss of jobs, school and daycare closures, and general uncertainties about the future may adversely impact individuals. Therefore, significant concern has developed regarding the potential mental health toll of the COVID-19 pandemic and has resulted in several studies examining the impact of the pandemic on mental well-being.
Several weeks after many states initiated lockdown measures, a cross-sectional internet-based survey was conducted and found high rates of depressive symptoms (47.3%) in the U.S. which were significantly elevated over the pre-pandemic baseline prevalence of 24%.12 Additionally, even after lockdowns were lifted, the prevalence of depressive symptoms remained elevated at 39%.13 However, the majority of studies to date have focused on the effects of the pandemic on the civilian population and have not directly evaluated the effects on the military population. Service members impaired by mental health conditions, such as depression, have a potential to endanger mission success during an era marked by the decreasing size of the active component military;14 therefore, identification of antecedents to depression, such as COVID-19, may help with efforts to mitigate their effects.
The main objective of this study was to assess the relationship between the COVID-19 pandemic and depressive symptoms in active component members of the U.S. military via two aims. The first aim was to determine whether the prevalence of depressive symptoms changed from the period prior to and during the COVID-19 pandemic. The second aim was to evaluate whether self-reported depressive symptoms were associated with recent SARS-CoV-2 infection.
Methods
The study population for the first aim included all active component U.S. military members in the Army, Navy, Air Force, or Marine Corps who completed a Periodic Health Assessment (PHA) between Jan. 1, 2019 and July 31, 2021. The study population for the second aim included all active component U.S. military members in the Army, Navy, Air Force, or Marine Corps who were tested for SARS-CoV-2 between Feb. 1, 2020 and Jan. 31, 2021.
PHA, demographic, and diagnosis data for this study were obtained from the Defense Medical Surveillance System (DMSS), which contains comprehensive longitudinal data and links demographic information to direct and Click to closePurchased CareThe TRICARE Health Program is often referred to as purchased care. It is the services we “purchase” through the managed care support contracts.purchased care health care encounters for active component service members of the U.S. Armed Forces. SARS-CoV-2 PCR and antigen test results were obtained from Composite Health Care System (CHCS) and from MHS GENESIS data extracts provided by the Epi Data Center at the Navy and Marine Corps Public Health Center.
Patient Health Questionnaire-2 (PHQ-2) Screening
Annually, each service member is required to complete a PHA which includes a validated 2-question depression screening instrument called the Patient Health Questionnaire-2 (PHQ-2).15 The questions ask participants to indicate how often over the last 2 weeks they have had the following problems: "Little interest or pleasure in doing things" and "Feeling down, depressed or hopeless." Each question is rated on a 4-point Likert scale with possible answers of "not at all" (0 points), "several days" (1 point), "more than half the days" (2 points), and "nearly every day" (3 points). A summed score of 3 points or greater is considered positive for depressive screening while a score of less than 3 points is negative.15
For the first study aim, the number of PHAs completed each month during the surveillance period were obtained. Any PHA record with an incomplete PHQ-2 was excluded from the study (0.11% of all PHA records in DMSS). Using a cut-off score of 3, each PHQ-2 was categorized as having screened positive for depression symptoms (hereafter referred to as "positive") or having screened negative for depression symptoms (hereafter referred to as "negative").15
SARS-CoV-2 Testing
For the second study aim, laboratory data were used to identify those who had completed a PCR test for SARS-CoV-2 during the surveillance period. Individuals who had a positive PCR test, a positive antigen test, a diagnosis of COVID-19 (International Classification of Diseases, 10th Revision [ICD-10]: U07.1), or a Disease Reporting System Internet (DRSi) record for COVID-19 confirmed or probable infection on any date prior to 1 Aug. 2021 were excluded from the negative test group. These individuals were included in the positive test group if they had a positive PCR test but were not included if they had a positive antigen test or COVID-19 diagnosis in the absence of a positive PCR test. If multiple PCR tests were found for the same individual within the study period, the test with a subsequent PHA within 28–180 days was used. If there was no PHA within this time period, the individual was excluded from this portion of the study. If there were multiple PCR/PHA pairs, the pair with a positive PHQ-2 was used and the others were excluded. If there were multiple pairs, but no positive PHQ-2, the pair with the earliest date was used.
Statistical Analyses
To evaluate for changes in depressive symptoms before and during the COVID-19 pandemic, the prevalence of screening positive for depression on the PHQ-2 was calculated for each month of the surveillance period and plotted. The percentage change in prevalence of positive PHQ-2s was further stratified by covariates of interest including age group, sex, military service, race/ethnicity group, military rank, marital status, education level, and military occupation.
For the second aim, demographic differences between the SARs-CoV-2 PCR positive and negative groups were assessed using Pearson's chi-square tests. Covariates included age group, sex, race/ethnicity group, military service, deployment status at the time of the SARS-CoV-2 test, and quarter/year of SARS-CoV-2 PCR testing. History of depressive disorder, as defined by the standard surveillance case definition used by the Armed Forces Health Surveillance Division (AFHSD), was evaluated as a potential effect modifier.16 Those who identified as an incident case of depression prior to the SARS-CoV-2 test date were considered to have a prior depressive disorder diagnosis. Additional variables included in this portion of the analysis were diagnosis of COVID-like illness (CLI), which was defined by having a CLI diagnosis within 10 days before or after the SARS-CoV-2 test in any diagnostic position of an inpatient, outpatient, or in-theater medical encounter; and hospitalization for COVID-19, which was defined by having a CLI diagnosis in the first or second diagnostic position of an inpatient encounter within 28 days after the SARS-CoV-2 test. To examine the relationship between the dichotomous variables of SARS-CoV-2 PCR status and PHQ-2 results, Poisson regression with robust error variance was used to generate crude and adjusted risk ratios (ARRs) and their associated 95% confidence intervals (CIs). The model adjusted for age group, sex, race/ethnicity group, service branch, education level, and quarter of the surveillance period. Analyses were conducted using SAS/STAT software, version 9.4 (2014, SAS Institute, Cary, NC).
Results
A total of 2,313,825 PHAs were completed from Jan. 1, 2019 to July 31, 2021 (data not shown). Of these PHAs, most were completed by male service members (82.3%), non-Hispanic White service members (55.9%), and enlisted members (80.8%). The largest percentage of PHAs were completed by members of the Army (40.2%), followed by Air Force (30.6%), Navy (17.9%) and Marine Corps (11.3%) (data not shown).
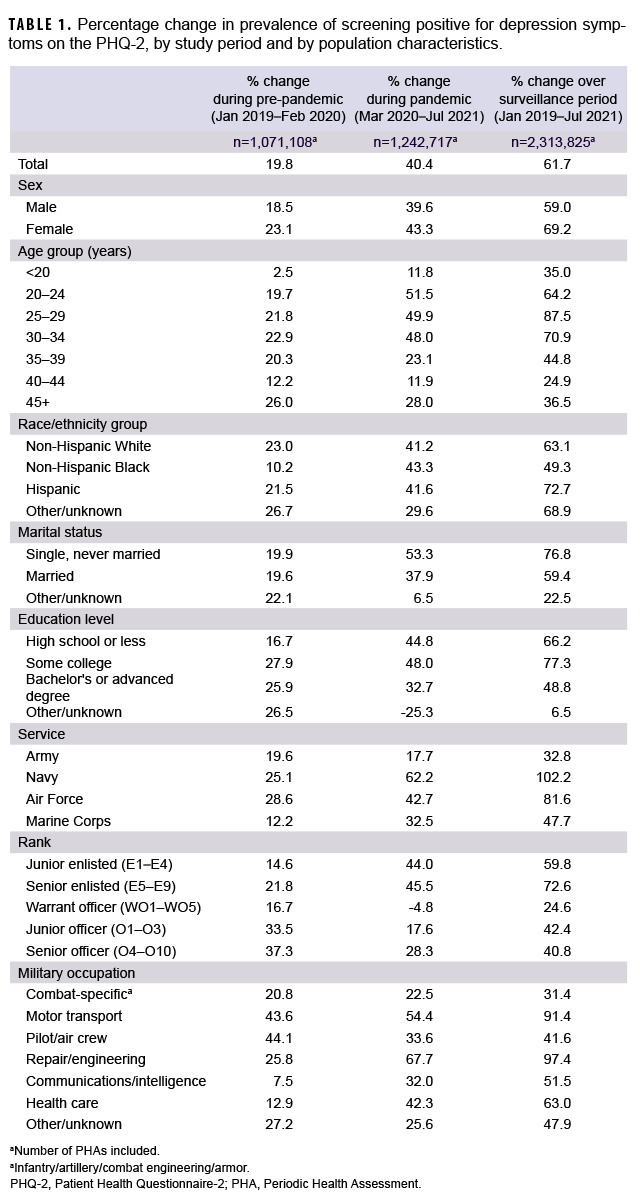
The overall monthly prevalence of positive PHQ-2s varied from 4.0% (Jan. 2019) to 6.5% (July 2021) with a relative % increase of 61.7% over the entire surveillance period (Figure). A gradual increase of 19.8% occurred between the beginning and the end of the pre-pandemic period (Jan. 2019–Feb. 2020) which was followed by a more pronounced increase of 40.4% during the pandemic period (March 2020–July 2021). The proportion of service members with positive PHQ-2s increased over the surveillance period for all subgroups examined. The greatest relative % increases from the beginning to the end of the period were seen in female service members (69.2%), those aged 25–29 (87.5%), Navy members (102.2%), Hispanics (72.7%), senior enlisted members (72.6%), those who were single, never married (76.8%), those who completed some college education (77.3%), and those in repair and engineering occupations (97.4%) (Table 1).
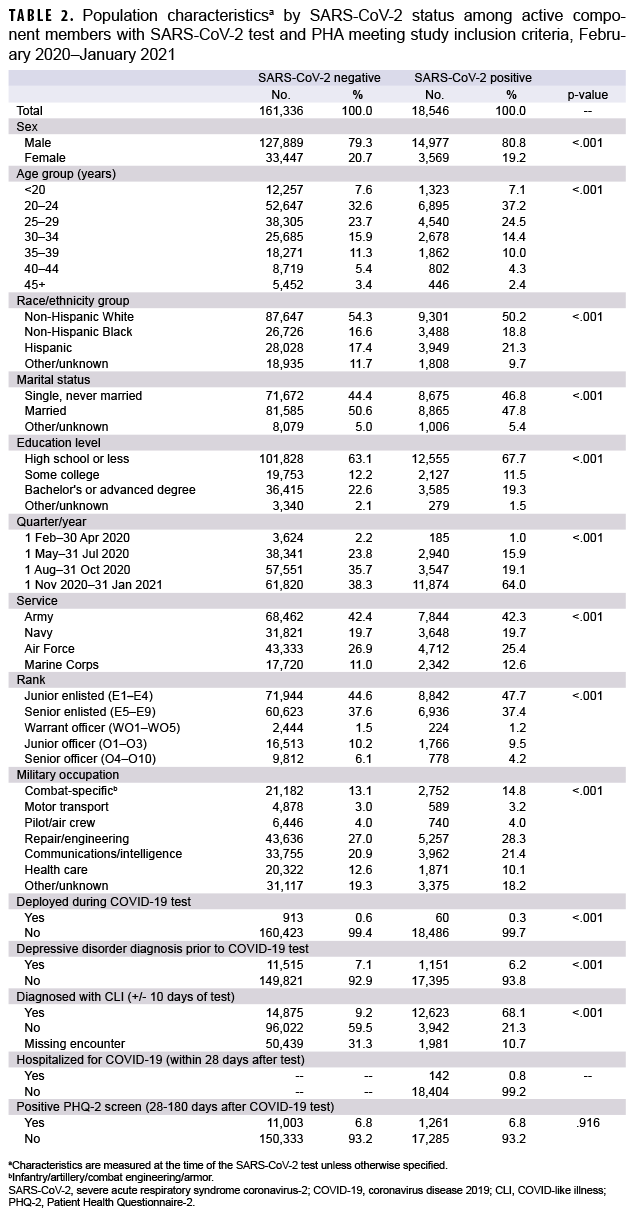
From Feb. 1, 2020 to Jan. 31, 2021, a total of 179,882 individuals were identified as having a SARS-CoV-2 PCR test results and PHAs that met the study inclusion criteria (Table 2). The percentage distributions in covariates were generally similar between the negative and positive test groups for most demographic categories. However, a few differences were noted: A higher percentage of individuals, aged 20–24, were in the SARS-CoV-2 positive group (37.2%) compared to the negative group (32.6%). Additionally, a higher percentage of non-Hispanic Whites were in the negative group compared to the positive group (54.3% vs. 50.2%), whereas a higher percentage of non-Hispanic Blacks (18.8%) and Hispanics (21.3%) were in the positive group compared to the negative group (16.6% and 17.4%, respectively).
Furthermore, a higher percentage of those with an education level of high school or less were in the positive group (67.7%) compared with the negative group (63.1%). In addition, a much higher percentage of positive tests were ascertained in the last quarter of the surveillance period compared to negative tests (64.0% and 38.3%, respectively). Finally, a much higher percentage of individuals in the positive test group were diagnosed with a CLI (68.1%) compared to those in the negative test group (9.2%). In both the negative and positive test groups, 6.8% screened positive on the PHQ-2 (Table 2), which exceeded the average prevalence of positive PHQ-2s in active component service members over the entire surveillance period (4.9%) and for every month during the surveillance period (range 4.1% to 6.5%) (data not shown).
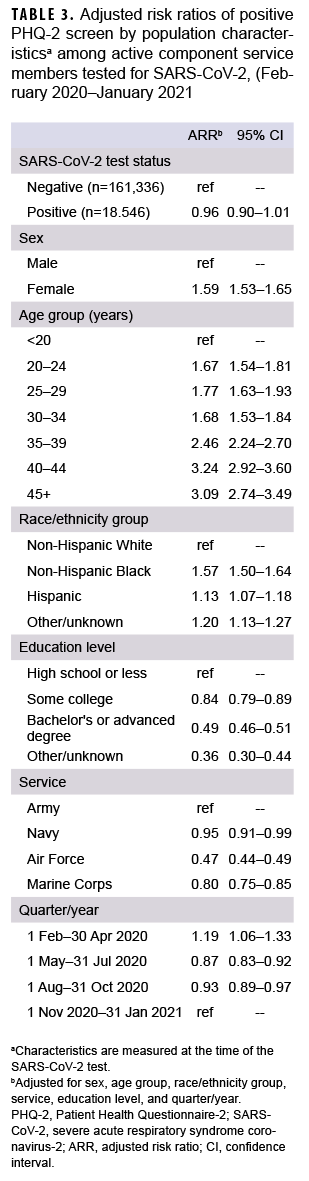
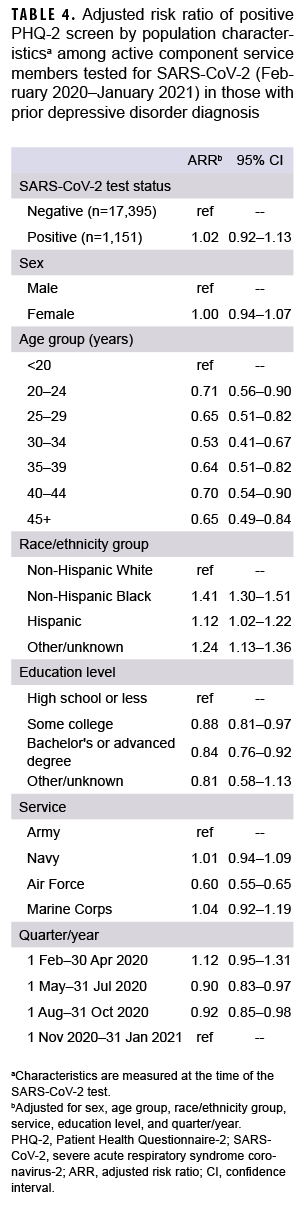
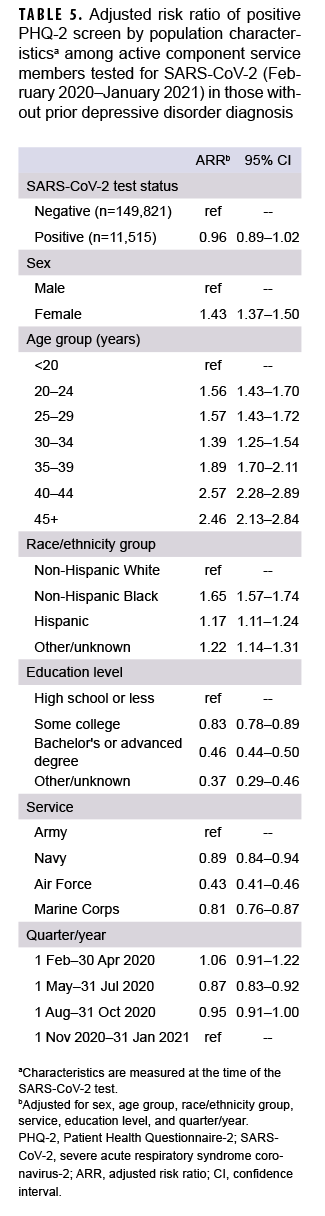
In both unadjusted and adjusted analyses, SARS-CoV-2 status was not associated with PHQ-2 result (RR=1.0; 95% CI: 0.94–1.05 [data not shown]; ARR=0.96; 95% CI: 0.91–1.01 [Table 3]). When the results were stratified by prior depressive disorder diagnosis, there was no statistically significant association between SARS-CoV-2 test result and screening positive on the PHQ-2 (with depressive disorder ARR=1.02; 95% CI=0.92–1.13 [Table 4]; without depressive disorder ARR=0.96; 95% CI=0.89–1.02 [Table 5]).
Editorial Comment
The prevalence of screening positive for depression symptoms on the PHQ-2 increased over the course of the surveillance period with the most pronounced increase during the COVID-19 pandemic period; however, the results of this study suggest that SARS-CoV-2 infection status is not associated with the presence of depressive symptoms among active component service members. In particular, members of the Navy, those aged 25–29, and those employed in repair and engineering occupations experienced the greatest increases in self-reported depressive symptoms over this period.
Between 2016 and 2020, the incidence of depressive disorders in active component service members, based on medical encounter data, remained fairly stable at an average of 214 per 10,000 person-years.17 The rate had decreased from 228.3 in 2019 to 211.6 in 2020 which differs from the findings in the current study that demonstrate an increase in depressive symptoms between 2019 and 2020;17 however, these rates cannot be directly compared as those diagnosed with depressive disorders likely have more severe symptomology than those screening positive for depressive symptoms. Additionally, the data collected on PHQ-2s is self-reported while a depression diagnosis results from a provider's clinical assessment. The overall decrease in the rate of depressive disorders diagnoses may be a function of the reduction in access to and use of medical services that occurred during the COVID-19 pandemic as opposed to an actual decrease in depressive disorders. The current study assessed responses on PHAs which are completed by service members online; therefore, completion of PHAs, and the PHQ-2s, included are less impacted by changes in access to care. In both prior analyses and the current study, the rates of depressive disorders and PHQ-2 positive screening results were highest in female service members, non-Hispanic Black service members, and enlisted members.
A key strength of this study is the large sample sizes of more than 2.3 million PHAs and nearly 180,000 SARS-CoV-2 tests. Additionally, this is one of the first studies to evaluate depressive symptoms associated with COVID-19 based on laboratory confirmed SARS-CoV-2 infection status. Misclassification of exposure (having or not having a SARS-CoV-2 infection) was minimized by the requirement that all individuals included in the study had a definitive SARS-CoV-2 test and result. Finally, this study used a validated depression screening instrument, the PHQ-2, as the outcome measure.
However, there are several limitations. First, underreporting of depressive symptoms on the PHQ-2 is likely. Due to the general stigma of mental health disorders and the specific military concern of a diagnosis with a mental health condition having an adverse impact on an individual's career, it is likely that many members underreport their symptoms on the PHQ-2. In the pilot/air crew field, this behavior is common as individuals endeavor to avoid any negative indicators that could result in their removal from flying duties. This is of significant concern in the diagnosis and treatment of depressive disorders; however, there is no evidence to suggest that the COVID-19 pandemic or being tested for SARS-CoV-2 would lead to a directional change in underreporting of symptoms on the PHQ-2; therefore, the misclassification bias is likely to be non-differential. Second, the study population is not perfectly representative of the overall active component service member population. Compared with 2019 active component demographic data, this study included a greater percentage of Air Force members, individuals over age 25, and those with bachelor's or advanced degrees while having a lower percentage of Navy members. The lower than expected percentage of Navy PHAs is likely related to the inability to include PHAs completed by sailors while at sea since these are not uploaded into DMSS. Additionally, due perhaps to a change in priorities of service members early in the pandemic, the number of PHAs completed from March through May 2020 decreased by approximately 25%; this change may have skewed the data, but would also be expected to result in non-differential misclassification bias.
Depression poses a significant threat to the U.S. military as it impairs the full medical readiness of personnel. This study demonstrates that the percentage of those screening positive for depressive symptoms was gradually increasing prior to the COVID-19 pandemic and that increase accelerated during the pandemic. While this rise is present across every demographic group, specific groups have experienced proportionally greater increases. Despite these increases, there was no association between SARS-CoV-2 test results and depressive symptoms and no evidence of a history of depression moderating this relationship. These results suggest that the increases in depressive symptoms are most likely a function of the environment of the COVID-19 pandemic instead of being due to the actual SARS-CoV-2 infection.
However, the positive PHQ-2 rate in those tested for SARS-CoV-2 exceeded the rate of the active component service member population at large. This suggests that concern about potential infection with SARS-CoV-2, and the resulting increased restrictions on social interaction, may have a greater influence on depressive symptoms than actually being diagnosed with SARS-CoV-2. It is vital that the military health system is equipped to quickly view and act on these results. Crucial to these efforts are the appropriate allocation of additional resources, such as staff and exam rooms, to manage the growing burden of depressive symptoms.
Further research is needed to more clearly understand these results and their impact on military members. Studies evaluating specific effects of the COVID-19 pandemic, such as fear of infection, school and daycare closures, social isolation, and the looming future uncertainty, are necessary to disentangle the relationship between the pandemic and depressive symptoms. Such studies can provide avenues for mitigation of depressive effects. More detailed depression tools evaluating disease severity, such as the PHQ-9, would help to determine the burden of disease. Additionally, research assessing the long-term impact of a positive PHQ-2 on a military member's career would assist with directing resources towards the areas of greatest need. To ensure the medical readiness of the U.S. military, evaluation and treatment of those suffering from depressive symptoms is essential.
Author affiliations: Department of Preventive Medicine and Biostatistics at the Uniformed Services University of the Health Sciences, Bethesda, MD (Dr. Smetana); Armed Forces Health Surveillance Division, Silver Springs, MD (Drs. Patel, Stahlman, Patel, Chauhan, Wells, and Ying).
Disclaimer: The opinions and assertions expressed herein are those of the author(s) and do not necessarily reflect the official policy or position of the Uniformed Services University or the Department of Defense.
References
- Rehm J, Shield KD. Global burden of disease and the impact of mental and addictive disorders. Curr Psychiatry Rep. 2019;21(2):10.
- Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: Results from the 2019 National Survey on Drug Use and Health. HHS Publication No. PEP20-07-01-001. Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; 2020.
- Villarroel MA, Terlizzi EP. Symptoms of depression among adults: United States, 2019. NCHS Data Brief, No. 379. Hyattsville, MD: Centers for Disease Control and Prevention, National Center for Health Statistics; 2020.
- Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: Results from the 2019 National Survey on Drug Use and Health. HHS Publication No. PEP20-07-01-001. Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; 2020.
- Villarroel MA, Terlizzi EP. Symptoms of depression among adults: United States, 2019. NCHS Data Brief, No. 379. Hyattsville, MD: Centers for Disease Control and Prevention, National Center for Health Statistics; 2020.
- Armed Forces Health Surveillance Division. DOD Health of the Force 2019. Accessed 28 Jan. 2022. https://www.health.mil/Military-Health-Topics/Combat-Support/Armed-Forces-Health-Surveillance-Division/Reports-and-Publications
- World Health Organization. Archived: WHO Timeline-COVID-19. Published June 29, 2020. Updated Dec. 28, 2020. Accessed Sept. 2, 2021. https://www.who.int/news/item/29-06-2020-covidtimeline
- Center for Systems Science and Engineering at Johns Hopkins University. COVID-19 Dashboard. Updated Aug. 17, 2021. Accessed Sept. 3, 2021.https://coronavirus.jhu.edu/map.html
- Defense Health Agency (DHA) Crisis Action Team. Assistant Director's Update Brief Event: COVID-19. Updated Sept. 1, 2021. Accessed Sept. 2, 2021.
- 10. Social Distancing. Centers for Disease Control and Prevention website. Updated Nov. 17, 2020. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/social-distancing.html
- Courtemanche C, Garuccio J, Le A, Pinkston J, Yelowitz A. Strong social distancing measures in the United States reduced the COVID-19 growth rate. Health Aff. 2020;39(7):1237–1246.
- Kantor BN, Kantor J. Mental health outcomes and associations during the COVID-19 pandemic: a cross-sectional population-based study in the United States. Front Psychiatry. 2020;11:569083.
- Khubchandani J, Sharma S, Webb FJ, Wiblishauser MJ., Bowman SL. Post-lockdown depression and anxiety in the USA during the COVID-19 pandemic. J Public Health (Oxf). 2021;43(2):246–253.
- U.S. military size 1985–2021. Macrotrends. Accessed 28 Aug. 2021. https://www.macrotrends.net/countries/USA/united-states/military-army-size
- Kroenke, K., Spitzer, R. L., & Williams, J. B. The patient health questionnaire-2: validity of a two-item depression screener. Med. Care. 2003;41(11):1284–1292.
- Armed Forces Health Surveillance Division. Surveillance Case Definition: Mental Health-Related Problems. February 2016. Accessed Jan. 28, 2022. https://www.health.mil/Military-Health-Topics/Combat-Support/Armed-Forces-Health-Surveillance-Division/Epidemiology-and-Analysis/Surveillance-Case-Definitions
- U.S. Department of Defense, Office of the Deputy Assistant Secretary of Defense for Military Community and Family Policy. 2019 Demographics: Profile of the Military Community. Accessed Sept. 2, 2021. https://download.militaryonesource.mil/12038/MOS/Reports/2019-demographics-report.pdf