Abstract
This study examined monthly prevalence of obesity and exercise in active component U.S. military members prior to and during the COVID-19 pandemic. Information about obesity (BMI≥30) and self-reported vigorous exercise (≥150 minutes per week) were collected from Periodic Health Assessment (PHA) data. From 1 January 2018 through 31 July 2021, there was a gradual increase in obesity and an overall decrease in vigorous exercise. Comparing the mean monthly percentage of obesity during the 12-month period prior to the pandemic to the 12 months after its start showed an overall increase in obesity (0.43%); however, no obvious spike in the obesity trend was apparent following the onset of the pandemic. The prevalence of vigorous exercise showed an abrupt decrease following the onset of the COVID-19 pandemic, but this change did not coincide with an abrupt change in the obesity trend. These results suggest that the COVID-19 pandemic had a small effect on the trend of obesity in the active component U.S. military and that obesity prevalence continues to increase.
What are the New Findings?
The prevalence of obesity in the military, as measured by the PHA, had been increasing prior to the pandemic and has continued to do so since the start of the pandemic. However, the onset of COVID-19 and the decline in self-reported exercise behaviors did not appear to have a large impact on the magnitude of the increasing trend in obesity prevalence.
What is the Impact on Readiness and Force Health Protection?
Understanding the impacts of COVID-19 lockdowns on fitness and health could assist in guiding policies to maintain health and readiness should future pandemics or societal disruptions occur.
Background
The increasing prevalence of obesity is a major problem affecting the overall and long-term health of the U.S. population. During 2017–2018, 42.4% of all U.S. adults met the threshold for obesity and 9.2% were classified as severely obese compared to 30.5% and 4.7% in 1999–2000, respectively.1 Obesity is responsible for an estimated $190 billion in excess medical costs and over 100,000 preventable cancer cases each year.2,3
The worsening trend of weight gain in the American public has also been reflected within the armed services. The overall prevalence of obesity within the active component increased from 16.3% in 2015 to 17.9% in 2019.4 As per Department of Defense Directive No. 1308.1, "Maintaining desirable body composition is an integral part of physical fitness, general health, and military appearance".5 Not only does obesity within the military ranks negatively impact the professional perception of the military, it also compromises its readiness and leads to functional limitations. For example, incidence of musculoskeletal injuries,6 excess health care utilization, and 90 day attrition have been found to be higher in overweight and obese service members and military recruits.7,8 In addition to various adverse physical effects, obesity is associated with multiple mental health disorders including depression, anxiety, and substance abuse disorders.9,10
The onset of the COVID-19 pandemic in March 202011 led to significant restrictions in activities that may have further exacerbated the worsening problem of obesity within the active military. This study sought to explore trends in population-level prevalence of obesity within the active component U.S. military population before and after the start of the COVID-19 pandemic. Investigations of the general public during COVID-19 have shown that members of certain demographic groups (race, ethnicity, age, and income) were more susceptible to weight gain during pandemic lockdowns.12 As pandemic and lockdown events continue to be a concern into the foreseeable future, evaluating multiple covariates within this population may help to identify certain groups that are more susceptible to weight gain under these conditions. Insight into this subject within the U.S. military could help inform the development of systems that maintain health and military readiness should any future societal disruptions occur.
For many reasons, the pandemic may have influenced obesity prevalence; they include halting of daily unit physical training, deferred physical fitness testing, and stay at home orders restricting non-essential movement. Not surprisingly, previous investigations into the overweight or obesity status of military personnel have shown vigorous exercise to be inversely associated with obesity,13 but there are other factors like overeating and stress that may have had an impact on service members' weights during this time.
Reducing attrition and retaining personnel is a constant problem for the armed services. Almost three-quarters (71%) of young adults in the U.S. between the ages of 17 and 24 do not meet requirements for military service because of inadequate educational attainment, overweight/obesity and other physical conditions, or history of criminal activity or illicit drug use.14 This concerning statistic highlights the importance of retaining qualified personnel, as the pool of qualified candidates has become increasingly smaller over time.
The overall objective of this study was to assess the relationship between COVID-19 and obesity prevalence in active component U.S. military members via 3 aims. The first aim was to determine the prevalence of obesity before and after the start of the COVID-19 pandemic. The second aim was to evaluate the trend of service member self-reported vigorous exercise during the COVID-19 pandemic. The third aim was to identify how many service members were separated from service due to obesity, with the goal of gauging the recent impact of obesity on attrition in the active component U.S. military and potentially identifying areas of focus to reduce weight gain and aid in service member retention.
Methods
The study population for this investigation included active component U.S. military members in the Army, Navy, Air Force, and Marine Corps who completed a Periodic Health Assessment (PHA) between Jan. 1, 2018 and July 31, 2021. PHA and demographic data were obtained from the Defense Medical Surveillance System (DMSS), which serves as the central repository of medical surveillance data for the U.S. Armed Forces. Women with a pregnancy/birth-related diagnosis (International Classification of Diseases, 10th Revision [ICD-10] code beginning with "O") in any diagnostic position in a record of an inpatient or outpatient encounter within 9 months of the date that their weight was recorded were excluded. Duplicate PHAs or those with listed weight more than 1 year old were also excluded.
Each service member is required to complete a PHA annually. Height (recorded in inches) and weight (recorded in pounds) data were obtained from Section II questions 2 and 3 of the PHA and are recorded by the service provider at the time of the PHA encounter, or derived from the patient medical record. Height and weight were subsequently used to calculate body mass index (BMI) using the formula: weight (lb) x 703/[height (in)]2.15 A service member with a BMI ≥30 was classified as obese.16 Records where weight was less than 40 lb or greater than 370 lb, height was less than 30 inches or greater than 100 inches, and where BMI was less than 12 or greater than 45 were excluded, as these measurements were assumed to be data entry errors.
Monthly PHA data on physical activity were obtained from the results of section VII question 6: "In a typical week, I do VIGOROUS physical activities (VIGOROUS activities cause HEAVY sweating or LARGE increases in breathing or heart rate) __ Days per week; __ Minutes per day on the days you do work out". Minutes per day of vigorous exercise was multiplied by days exercised per week to determine total minutes per week of vigorous exercise. All military service members are expected to exercise 5 days a week as part of their duty requirements. For the purpose of this study, those service members endorsing 30 minutes of vigorous intensity exercise 5 times a week (totaling 150 minutes) were considered to have met vigorous exercise requirements. Service members on a profile limiting their ability to participate fully in a physical fitness test were identified by a "yes" response on section IV question 8.a. of the PHA "Do you currently have a waiver or profile for any part of your Service's physical fitness test?"
DMSS data were used to identify individuals separated from service using interservice separation codes (ISC) 1017 and 2017 (failure to meet weight or body fat standards). Those who had their weight recorded between Jan. 1, 2018 and Dec. 31, 2019 and were classified as obese were followed through the latest date that separation data were available, which was Aug. 31, 2021 at the time of the analysis. In addition, the median number of days since diagnosis of obesity was summarized and stratified by sex, age group, military service branch, race/ethnicity group, rank, marital status, education level, military occupation, geographic region at the time of the weight measurement, and whether the service member had a waiver or profile for any part of the physical fitness test reported at the time of the PHA.
To assess trends in prevalence of obesity within the active component U.S. military population before and during the COVID-19 pandemic, the prevalence of obesity for each month in the surveillance period was calculated using the date of the weight measurement. In addition, trends were stratified by presence of fitness test limiting profile and self-reported weekly vigorous exercise of at least 150 minutes/week. Among the service members who completed a PHA between Aug. 1, 2020 and July 31, 2021, prevalence of obesity was calculated for each of the covariates of interest to determine which subgroups were more or less likely to be obese. Mean change in monthly prevalence of obesity was also calculated by subtracting the mean monthly obesity prevalence during the 1-year period prior to the declaration of the pandemic (March 2019–February 2020) from the 1-year period after the start of the pandemic (March 2020–February 2021).
Results
A total of 2,948,625 PHAs were completed from Jan. 1, 2018 through July 31, 2021. Of these completed assessments, 315,960 (10.7%) contained missing or invalid BMI values and were excluded (data not shown). The majority of PHAs (84.3%) were completed by male service members and 15.6% were completed by female service members, which closely approximates the sex distribution of the active component. The population of service members who completed PHAs during the surveillance period also closely approximated estimates of the active component overall in terms of marital status, education level, rank, and age.17 However, the Navy was underrepresented in the population of service members who completed PHAs; Navy members made up 17.5% of the study population compared to 25.1% of the total population of active component service members in 2019.17
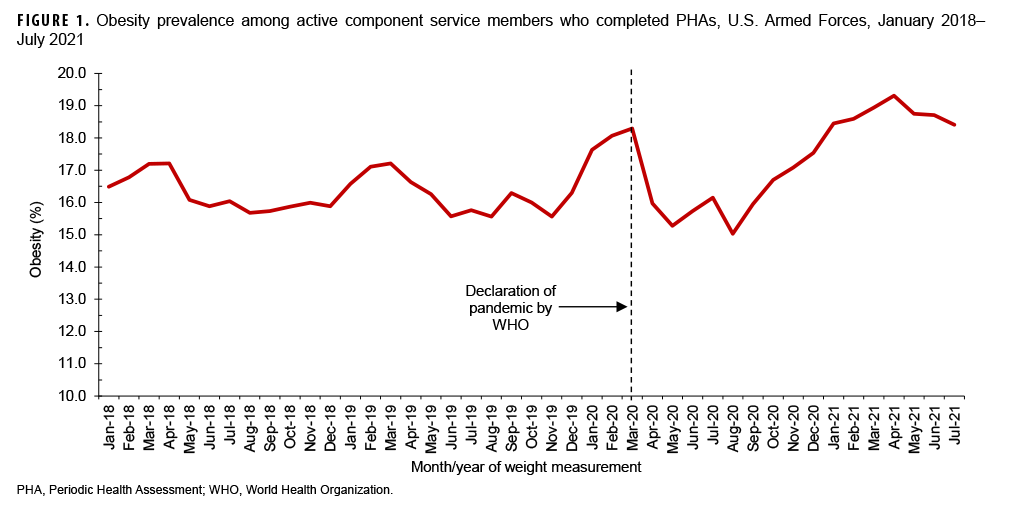
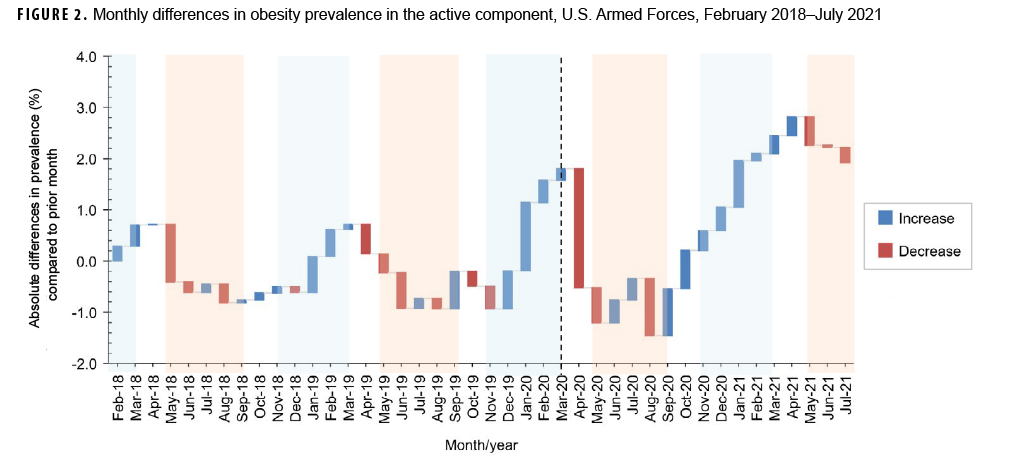
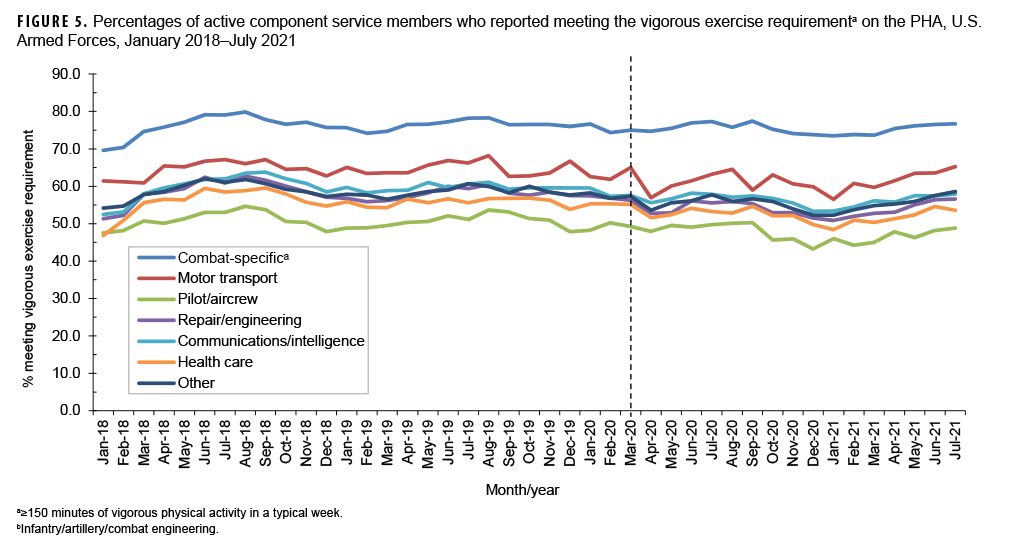
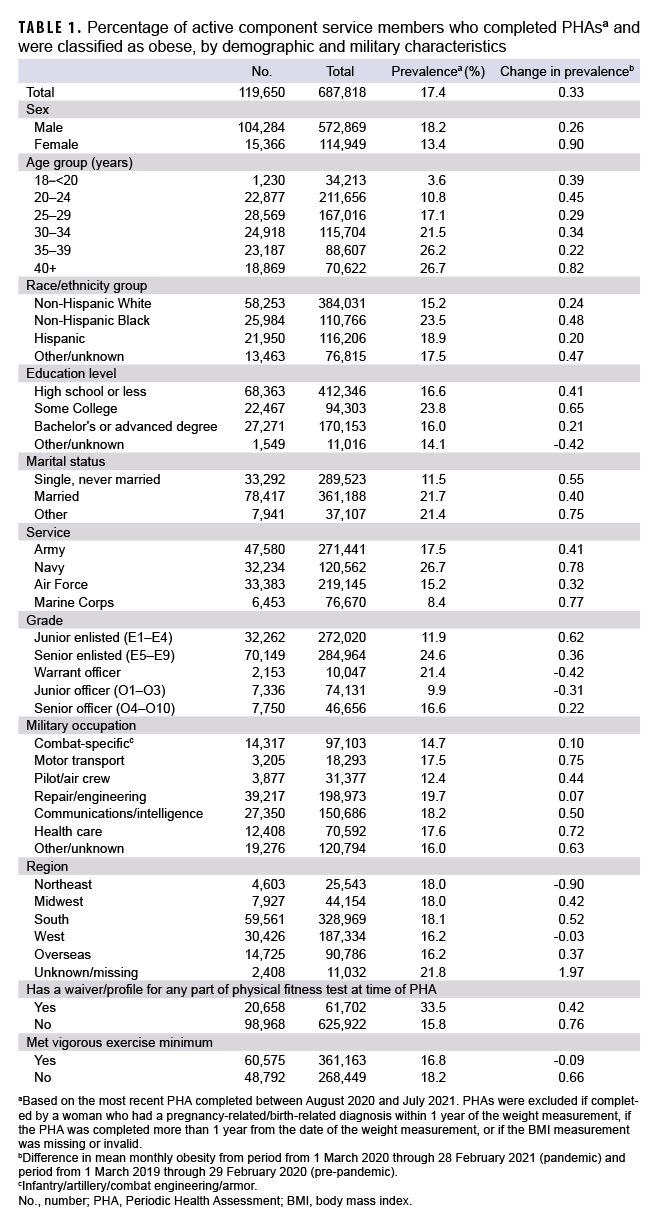
During the study period, the monthly prevalence of obesity ranged from a low of 15.0% in August 2020 to a high of 19.3% in April 2021 with substantial fluctuations by month throughout the period (Figure 1). There was a 0.33% absolute increase in mean monthly obesity prevalence between the 12-month period prior to the pandemic and the 12 months after the start of the pandemic (Table 1). Examination of the consecutive monthly absolute differences in obesity prevalence over time showed seasonal patterns with consecutive monthly increases in obesity prevalence generally occurring during winter months and consecutive monthly decreases tending to occur in summer months (Figure 2). Among female service members, the absolute difference between the mean monthly obesity prevalence during the pandemic period and the pre-pandemic period was 0.90% compared to a 0.26% rise in men (Table 1). Among the services, the Navy and Marine Corps demonstrated the largest absolute increase in mean monthly obesity prevalence from the pre-pandemic period to the pandemic period (0.78% and 0.77%, respectively). Compared to their respective counterparts, other relatively high absolute increases in mean monthly obesity prevalence occurred among service members aged 40 years or older (0.82%), non-Hispanic Black service members (0.48%), junior enlisted members (0.62%), those with "other" marital status (0.75%), and those with an occupation in motor transport (0.75%) (Table 1).
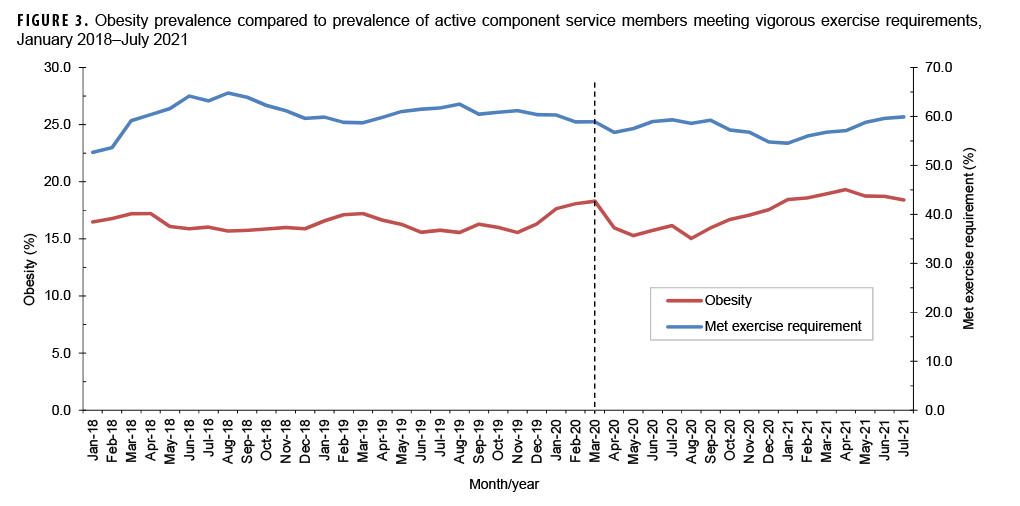
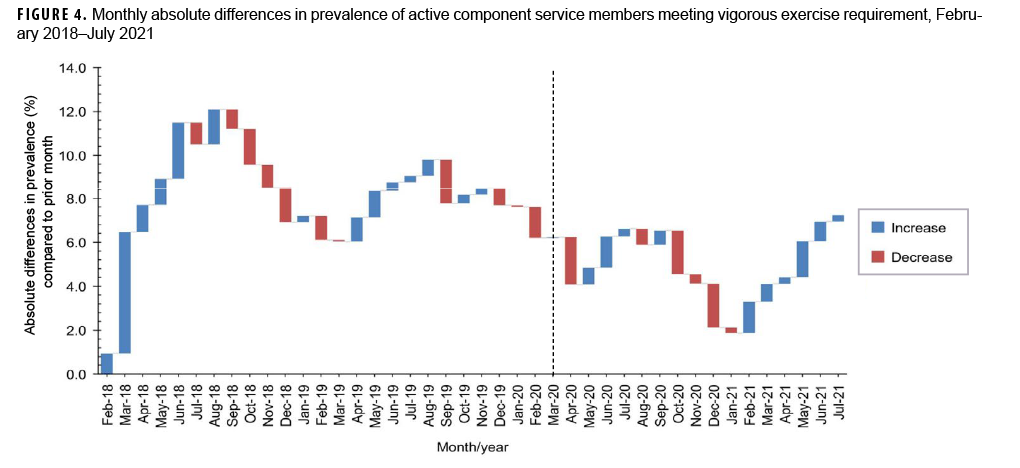
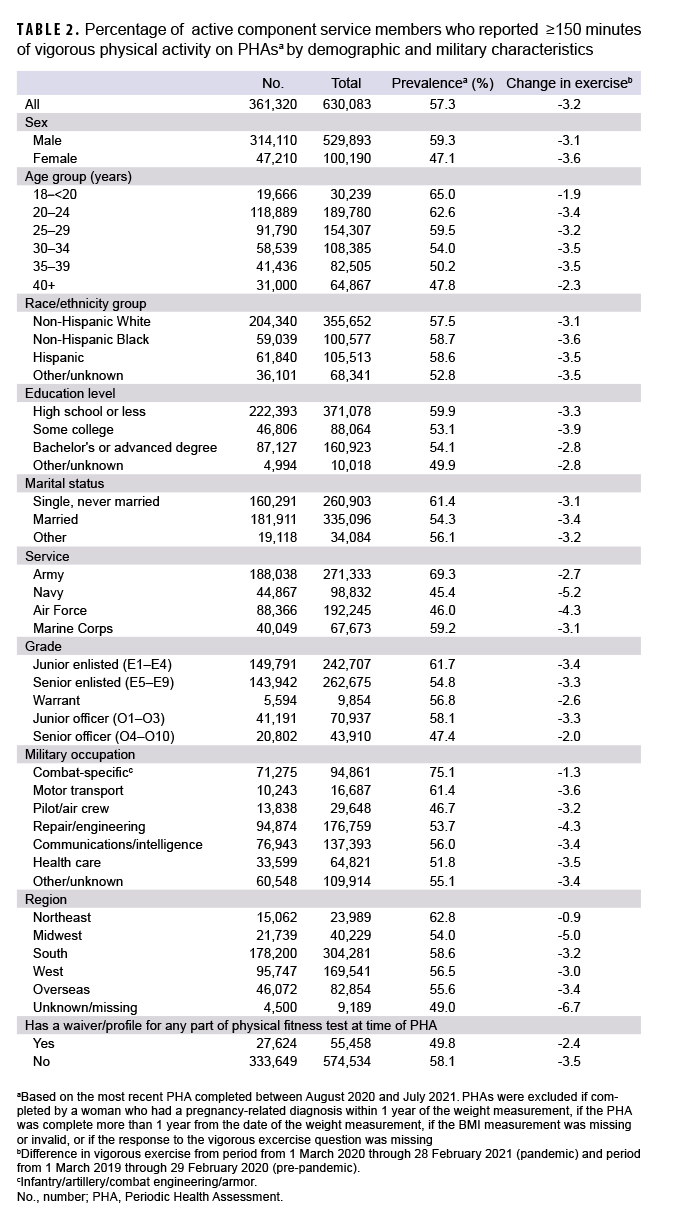
The percentage of active component service members reporting vigorous exercise fluctuated throughout the surveillance period and did not coincide with a shift in the overall obesity trend (Figure 3). Evaluation of the consecutive monthly absolute differences in vigorous exercise over time showed seasonal patterns where vigorous exercise prevalence tended to have consecutive monthly increases beginning in early spring and consecutive monthly decreases beginning in early fall (Figure 4). Comparison of the average monthly prevalence of vigorous exercise in the 12 months before and after the start of the pandemic demonstrated that vigorous exercise decreased variably across the service branches with the Navy showing the greatest absolute decrease of 5.2% (Table 2). Active component service members in combat-specific occupations displayed fewer fluctuations over time in the percentages meeting the vigorous exercise requirement compared to those in other occupational groups (Figure 5). Exercise trends by age group, rank, sex, race/ethnicity group, and service branch were similar throughout the surveillance period (data not shown).
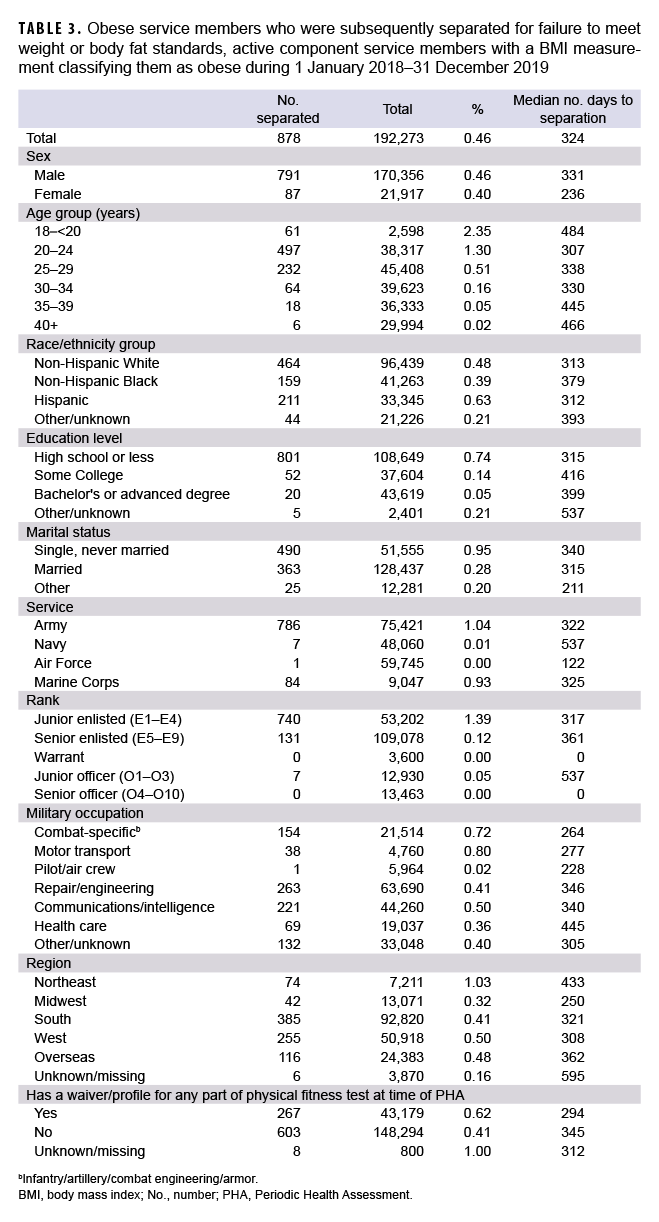
A total of 878 service members (0.46%) who had their weight measured between Jan. 1, 2018 and Dec. 31, 2019 were separated from service by August 2021 for failure to meet weight or body fat standards (Table 3). The median time from being classified as obese to separation from military service was 324 days. Higher percentages of obese active component service members aged 18–20 (2.35%) and 20–24 (1.30%) were separated because of obesity compared to older service members, especially those aged 40 or older (0.02%). Junior enlisted personnel were more likely to be separated for obesity (1.39%) compared to senior enlisted (0.12%) or junior officers (0.05%), and there were no senior officers (O4–O10) or warrant officers separated during the study period. Army and Marine Corps members were more likely to be separated for obesity, at 1.04% and 0.93%, respectively, compared to <0.01% in the Air Force and the Navy.
Editorial Comment
The trends identified in this study suggest that the COVID-19 pandemic may have been associated with an increase in obesity prevalence among active component service members, but it was not an immediate abrupt jump in obesity prevalence. Instead, the steadily increasing trend of obesity that occurred prior to the pandemic continued with only a modest increase beginning in August 2020. Given the abrupt implementation of COVID-19 restrictions, which included the closing of gyms and parks, modification of many military base operations, as well as an increase in alcohol consumption, screen time, and decreased exercise among U.S. adults,18 a larger increase in the prevalence of obesity might have been expected.
Examination of trends in the prevalence of obesity and percentages of active component service members meeting minimum exercise requirements revealed cyclical patterns. During the pre-pandemic period, obesity prevalence generally peaked in March and April followed by pronounced drops in the summer months. This pattern was even more pronounced after the start of the pandemic with obesity prevalence peaking in April 2021 at a level higher than at any point during in the pre-pandemic period.
A potential explanation for this pattern could be seasonal behaviors following the holiday and Permanent Change of Station (PCS) seasons that lead to service members gaining weight and subsequently dropping weight afterwards in order to pass biannual testing for height and weight. Prevalence of vigorous exercise, on the other hand, increased in the early spring and peaked at the start of fall, which may be reflective of changes in the ambient temperature and outdoor exercise conditions. Service members in combat-specific occupations, who are most strictly held to daily physical training regimens as part of their profession, showed the least seasonal change in exercise compared to other service members, further supporting this explanation.
There have been few studies in adults studying the longitudinal effects of the COVID-19 pandemic on obesity, but a study of the civilian U.S. population evaluating 2–20 year-olds showed an increase in obesity in all age groups evaluated.19 Though there are substantial differences in the ages and health profiles of these populations, this investigation showed similar findings with subjects in every age category showing increased prevalence of obesity secondary to the pandemic. Military members continue to maintain obesity levels well below their respective civilian counterparts;1 however, the continued rise in obesity in the military is concerning.
Younger and lower ranking service members were more likely to be separated for failure to meet height/weight standards. One explanation for this could be that those service members who screened positive for obesity at an earlier point in their careers are more likely to fail verification via service-specific body measurements ("tape testing") compared to those who have served longer. It is also possible that higher ranking individuals with more time in service are less easily replaceable and therefore less likely to have this standard applied for separation due to manning concerns. Considering they had just recently met height and weight standards to qualify for accession, this raises the possibility that better instilling good exercise and dietary habits in young service members could lead to better overall retention of this subgroup.
This is one of the first studies to evaluate obesity trends in the military in the context of COVID-19. However, there are several limitations that should be considered when interpreting the results. First, BMI calculations do not account for variability in body type or muscular composition, especially in a young athletic population; therefore, BMI measurements use can lead to misclassification bias in favor of obesity, but these instances are rare. More accurate reporting of obesity could be performed by using results from each service's follow-on body composition testing; however, these data were not available for this study. Second, service members' vigorous exercise results were based on self-reporting and did not include moderate exercise, so the estimates presented here may not be an accurate representation of total physical exertion.
Future studies could consider studying a retrospective cohort of service members who became obese during the pandemic to identify specific risk factors for weight gain, as this could help to elucidate trends that were difficult to detect on a population level via this study of cross-sectional monthly prevalence. Such a study design would allow for examination of factors like dietary intake, and alcohol and tobacco consumption, all of which may have changed during the pandemic.18 The evidence of the cyclic trends of obesity and exercise also warrants further investigation as these patterns may reveal a failure to maintain accountability of service members' fitness outside of the times when physical fitness testing is performed. Identifying ways to improve consistent behaviors throughout the year may help to stem the increasing levels of obesity observed in the military. If this increasing obesity trend continues, current anti-obesity initiatives including utilization of wellness centers, dietary options in base dining facilities, and hours restricting access to exercise facilities should be re-examined to better tackle this problem.
Disclaimer: The views expressed in this article are those of the authors and do not necessarily reflect the official policy of the Department of Defense or the U.S. Government.
Author affiliations: Department of Preventive Medicine & Biostatistics, Uniformed Services University, Bethesda, MD (MAJ Legg); Defense Health Agency, Armed Forces Health Surveillance Division, Silver Spring, MD (Dr. Stahlman, Dr. Chauhan, Dr. Patel, Ms. Hu, and CAPT Wells).
References
1. Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of obesity and severe obesity among adults: United States, 2017–2018. NCHS Data Brief. 2020(360):1–8.
2. Arnold M, Pandeya N, Byrnes G, et al. Global burden of cancer attributable to high body-mass index in 2012: a population-based study. Lancet Oncol. 2015;16(1):36–46.
3. Cawley J, Meyerhoefer C. The medical care costs of obesity: an instrumental variables approach. J Health Econ. 2012;31(1):219–230.
4. Armed Forces Health Surveillance Division. Department of Defense Health of the Force 2019. 2020. Accessed 4 November 2021. https://www.health.mil/Military-Health-Topics/Combat-Support/Armed-Forces-Health-Surveillance-Division/Reports-and-Publications
5. Department of Defense. Directive Number 1308.1 DoD Physical Fitness and Body Fat Programs. 30 June 2004.
6. Dos Santos Bunn P, de Oliveira Meireles F, de Souza Sodre R, Rodrigues AI, da Silva EB. Risk factors for musculoskeletal injuries in military personnel: a systematic review with meta-analysis. Int Arch Occup Environ Health. 2021;94(6):1173–1189.
7. Krauss MR, Garvin NU, Boivin MR, Cowan DN. Excess stress fractures, musculoskeletal injuries, and health care utilization among unfit and overweight female Army trainees. Am J Sports Med. 2017;45(2):311–316.
8. Cowan DN, Bedno SA, Urban N, Yi B, Niebuhr DW. Musculoskeletal injuries among overweight army trainees: Incidence and health care utilization. Occup Med (Lond). 2011;61(4):247–252.
9. Petry NM, Barry D, Pietrzak RH, Wagner JA. Overweight and obesity are associated with psychiatric disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychosom Med. 2008;70(3):288–297.
10. Rivenes AC, Harvey SB, Mykletun A. The relationship between abdominal fat, obesity, and common mental disorders: results from the HUNT study. J Psychosom Res. 2009;66(4):269–275.
11. World Health Organization. Archived: WHO Timeline-COVID-19. Accessed 4 November 2021. https://www.who.int/news/item/29-06-2020-covidtimeline.
12. Jenssen BP, Kelly MK, Powell M, Bouchelle Z, Mayne SL, Fiks AG. COVID-19 and changes in child obesity. Pediatrics. 2021;147(5):e2021050123..
13. Reyes-Guzman CM, Bray RM, Forman-Hoffman VL, Williams J. Overweight and obesity trends among active duty military personnel: a 13-year perspective. Am J Prev Med. 2015;48(2):145–153.
14. Council for a Strong America; 2020. Breaking Point: Child malnutrition imperils America's national security. Accessed 10 October, 2021.c https://www.cdc.gov/obesity/adult/defining.html
15. Centers for Disease Control and Prevention. Healthy Weight, Nutrition, and Physical Activity. About Adult BMI. Accessed 4 November 2021. https://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html
16. Centers for Disease Control and Prevention. Overweight & Obesity. Defining Adult Overweight & Obesity. Accessed 27 September 2021. https://www.cdc.gov/obesity/adult/defining.html
17. Department of Defense, Office of the Deputy Assistant Secretary of Defense for Military Community and Family Policy (ODASD (MC&FP)). 2019. Demographics: Profile of the Military Community. 2020.
18. Chen L, Li J, Xia T, et al. Changes of exercise, screen time, fast food consumption, alcohol, and cigarette smoking during the COVID-19 pandemic among adults in the United States. Nutrients. 2021;13(10):3359.
19. Lange SJ, Kompaniyets L, Freedman DS, et al. Longitudinal trends in body mass index before and during the COVID-19 pandemic among persons aged 2–19 years - United States, 2018–2020. MMWR Morb Mortal Wkly Rep. 2021;70(37):1278–1283.