What Are the New Findings?
Musculoskeletal disorders and mental health disorders accounted for more than half (52.6%) of all illness- and injury-related ambulatory encounters among active component service members in 2018. Since 2014, the number of ambulatory visits for mental health disorders has decreased, while the numbers of ambulatory visits for musculoskeletal system/connective tissue disorders, nervous system and sense organ disorders, and respiratory system disorders have increased.
What Is the Impact on Readiness and Force Health Protection?
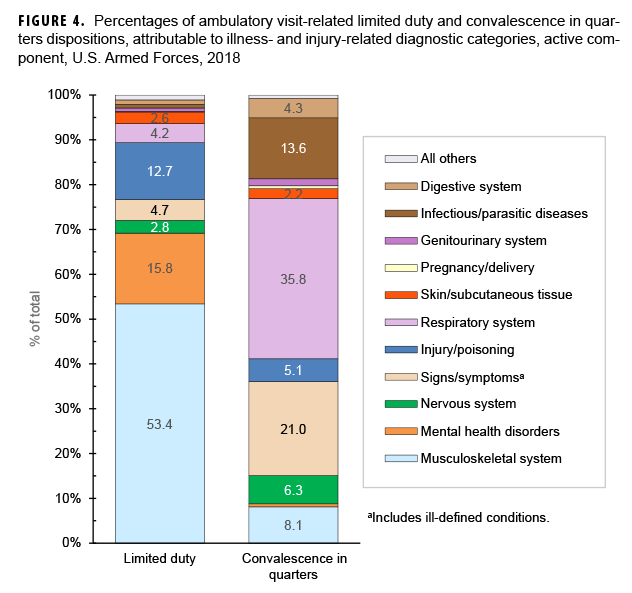
Ambulatory visits for injury/poisoning and musculoskeletal system disorders resulted in the largest percentages of limited duty dispositions among service members diagnosed in military treatment facilities. Duty limitations adversely affect the readiness of affected service members' units. Prevention and treatment of the most common causes of duty limitations will help preserve units' readiness.
Background
This report documents the frequencies, rates, trends, and characteristics of ambulatory health care visits of active component members of the U.S. Army, Navy, Air Force, and Marine Corps during 2018. Ambulatory visits of U.S. service members in fixed military and nonmilitary (reimbursed through the Military Health System [MHS]) medical treatment facilities are documented with standardized, automated records. These records are routinely archived for health surveillance purposes in the Defense Medical Surveillance System (DMSS), which is the source of data for this report. Ambulatory visits that are not routinely and completely documented with standardized electronic records (e.g., during deployments, field training exercises, or at sea) are not included in this analysis. As in previous MSMR reports, all records of ambulatory visits of active component service members were categorized according to the first 4 characters of the International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) codes entered in the primary (first-listed) diagnostic position of the visit records.1 The analysis depicts the distribution of diagnoses according to the 17 traditional categories of the ICD system.
Frequencies, Rates, and Trends
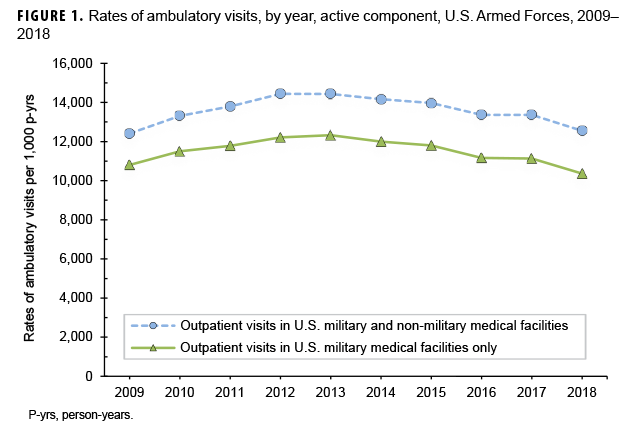
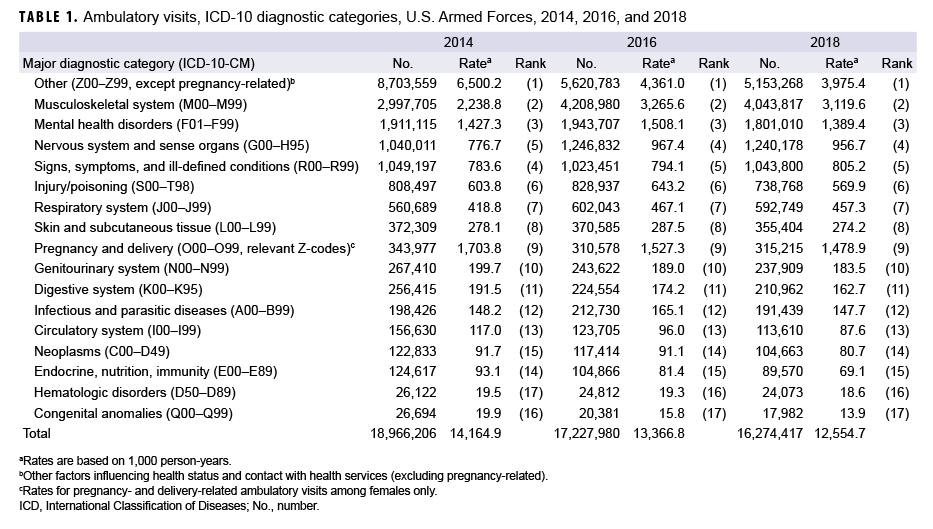
During 2018, there were 16,274,417 reported ambulatory visits of active component service members. The crude annual rate (all causes) was 12,554.7 visits per 1,000 person-years (p-yrs) or 12.6 visits per p-yr; thus, on average, each service member had approximately 13 ambulatory encounters during the year (Table 1). The rate of documented ambulatory visits in 2018 (12,554.69 per 1,000 p-yrs) was 6.1% lower than the rate in 2016 (13,366.8 visits per 1,000 p-yrs) and 13.0% lower than the peak in 2012 (14,438.9 visits per 1,000 p-yrs) but 1.2% higher than in 2009 (12,411.3 per 1,000 p-yrs) (Figure 1). In 2018, 31.7% of ambulatory visits were classified into the "other" category (i.e., other factors influencing health status and contact with health services, excluding pregnancy-related), which includes health care not related to a current illness or injury (Table 1). Such care includes counseling, immunizations, deployment-related health assessments, routine and special medical examinations (e.g., periodic, occupational, or retirement), and therapeutic and rehabilitative treatments for previously diagnosed illnesses or injuries (e.g., physical therapy).
In 2018, there were 11,121,149 documented ambulatory visits for illnesses and injuries (ICD-10: A00–T88, including relevant pregnancy Z-codes), not including diagnoses classified as "other" (Table 1). The crude annual rate of illness- and injury-related visits was approximately 8.6 visits per p-yr. The rate of ambulatory visits for illnesses and injuries in 2018 (8.6 visits per p-yr) was similar to the rate in 2016 (9.0 visits per p-yr) but slightly higher than the rate in 2014 (7.7 visits per p-yr).
Ambulatory Visits, by Diagnostic Categories
In 2018, 4 major diagnostic categories accounted for 73.1% of all illness- and injury-related ambulatory visits among active component service members: musculoskeletal system/connective tissue disorders (36.4%); mental health disorders (16.2%); disorders of the nervous system and sense organs (11.2%); and signs, symptoms, and ill-defined conditions (9.4%) (Table 1).
Between 2014 and 2018, there were increases in the numbers of visits in 3 major diagnostic categories of illness and injury and decreases in 13 categories (Table 1). The largest percentage increases in ambulatory visits during 2014–2018 were for musculoskeletal system/connective tissue disorders (change: +1,046,112 visits; +34.9%) and disorders of the nervous system and sense organs (change: +200,167; +19.2%). The largest decrease in numbers of visits between 2014 and 2018 was for mental health disorders (change: -110,105; -5.8%). The largest percentage decreases in ambulatory visits during 2014–2018 were for congenital anomalies (change: -8,712; -32.6%); endocrine, nutrition, and immunity disorders (change: 35,047; -28.1%); disorders of the circulatory system (change: -43,020; -27.5%); and disorders of the digestive system (change: -45,453; -17.7%). Moreover, the rates of ambulatory visits for illnesses and injuries in these categories showed consistent decreases during the 5-year period.
Over 5-year surveillance period, the relative distributions of ambulatory visits by the ICD-10 diagnostic categories remained stable with a few exceptions (Table 1). In a comparison of the numbers and rates of visits attributable to each of the 17 major diagnostic categories in the years 2014 and 2018, the rank orders of 3 pairs of categories were exchanged: disorders of the nervous system and sense organs (5th to 4th) and signs, symptoms, and ill-defined conditions (4th to 5th); neoplasms (15th to 14th) and endocrine, nutrition, and immunity disorders (14th to 15th); and hematologic and immune system disorders (17th to 16th) and congenital anomalies (16th to 17th). The rank orders of the major diagnostic categories (including "other") were the same in 2016 and 2018.
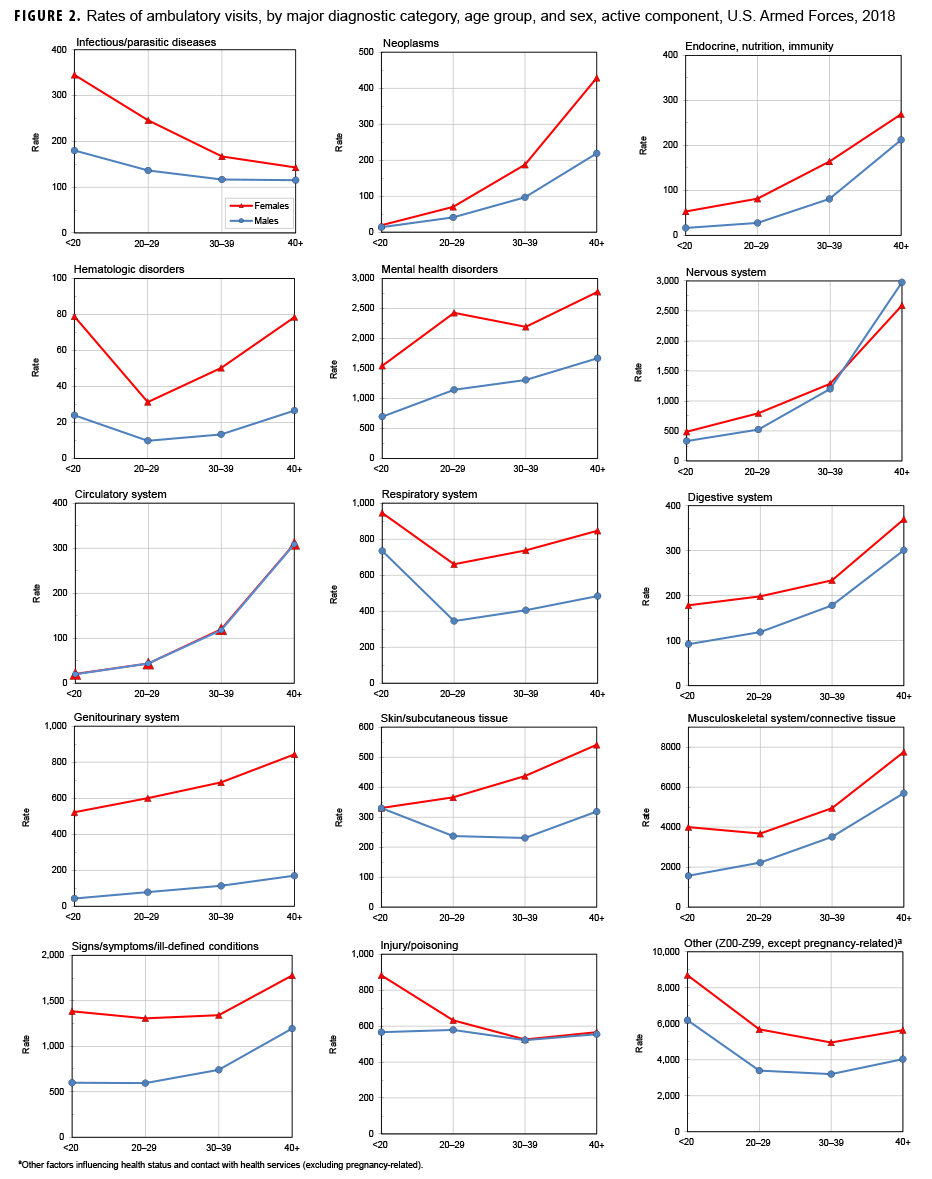
Ambulatory Visits, by Sex
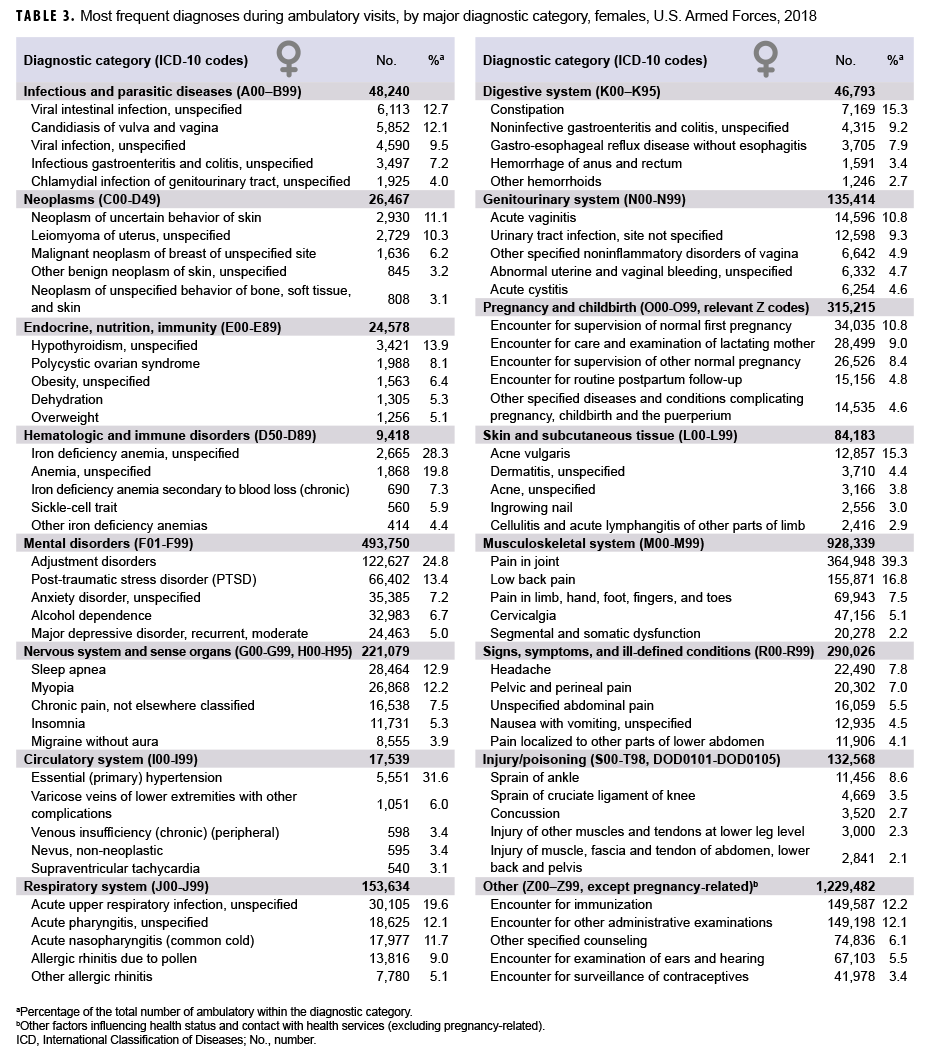
In 2018, males accounted for nearly three-fourths (73.6%) of all illness- and injury-related visits; however, the annual crude rate among females (13.8 visits per p-yr) was 81.9% higher than that among males (7.6 visits per p-yr) (data not shown). Excluding pregnancy- and delivery-related visits (which accounted for 10.8% of all non-Z-coded ambulatory visits among females), the illness and injury ambulatory visit rate among females was 12.3 visits per p-yr. As in the past, rates were higher among females than males for every illness- and injury-related category except circulatory disorders (Figure 2).
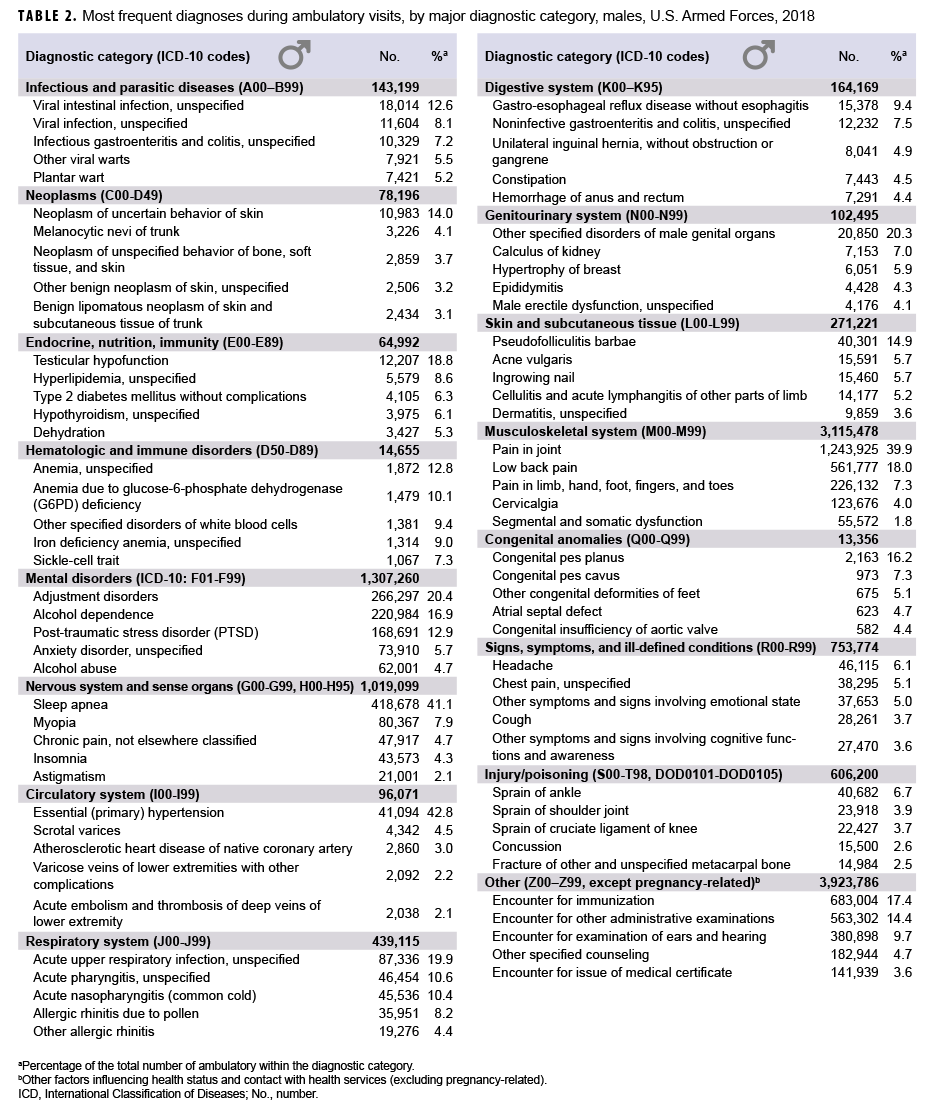
Among all illness- and injury-specific diagnoses, 3 of the 5 diagnoses with the largest numbers of ambulatory visits were the same for males and females. However, the crude rate (per 1,000 p-yrs) was at least 41% higher among females than males for these 3 common diagnoses: pain in joint (female: 1,712.2; male: 1,148.4; female:male rate ratio [RR]: 1.49), low back pain (female: 731.3; male: 518.1; RR: 1.41), and adjustment disorders (female: 575.3; male: 245.9; RR: 2.34) (data not shown). Five other diagnoses were among the 10 most common diagnoses for both males and females: alcohol dependence; pain in limb, hand, foot, fingers, and toes; post-traumatic stress disorder (PTSD); cervicalgia; and acute respiratory infection, unspecified. Of note, sleep apnea was the 3rd most frequent illness- or injury-specific primary diagnosis during ambulatory visits of males, but it ranked as the 12th most common diagnosis among females. Among females, the 7th most common diagnosis was anxiety disorder, unspecified, which was the 11th most common diagnosis among males (Tables 2, 3).
Across diagnostic categories, relationships between age group and ambulatory visit rates were broadly similar among males and females (Figure 2). For example, among both males and females, ambulatory visit rates for neoplasms and circulatory disorders among those aged 40 years or older were 15 or more times the rates among those younger than 20 years old; in contrast, clinic visit rates for infectious and parasitic diseases were lower among the oldest compared to the youngest service members. As in the past, ambulatory visit rates for disorders of the nervous system; digestive system; endocrine, nutrition, and immunity system; and musculoskeletal system rose more steeply with advancing age than most other categories of illness or injury (for which rates were relatively stable or only modestly increased) (Figure 2).
Dispositions After Ambulatory Visits
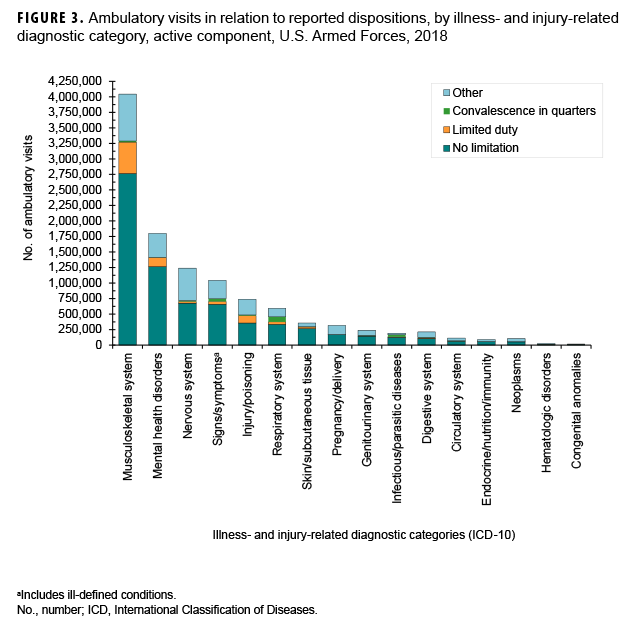
Because disposition codes are assigned to ambulatory medical encounters that occur only at military treatment facilities (MTFs), the following metrics do not include outsourced care. Approximately 63.4% of all illness- and injury-related visits resulted in "no limitation" (i.e., duty without limitations) dispositions (data not shown). Approximately 1 in 48 (2.1%) illness- and injury-related visits resulted in "convalescence in quarters" dispositions (data not shown). The illness- and injury-related diagnostic categories with the highest proportions of "limited duty" dispositions were injury/poisoning (16.3%) and musculoskeletal system disorders (12.5%) (Figure 3). The illness- and injury-related diagnostic categories with the highest proportions of "convalescence in quarters" were infectious/parasitic diseases (16.2%) and diseases of the respiratory system (13.8%). Musculoskeletal system/connective tissue disorders (53.4%) accounted for more than half of all "limited duty" dispositions, and mental health disorders (15.8%) and injury/poisoning (12.7%) together accounted for more than one-quarter (28.5%) (Figure 4). Diseases of the respiratory system accounted for more than one-third (35.8%) of all "convalescence in quarters" dispositions—more than twice as many (n=81,556) as any other disease category, except signs and symptoms (21.0%).
Editorial Comment
Over the 5-year surveillance period, the distribution of illness- and injury-related ambulatory visits in relation to their reported primary causes has remained fairly stable. In 2018, musculoskeletal system and mental health disorders accounted for more than one-half (52.6%) of all illness- and injury-related diagnoses documented on standardized records of ambulatory encounters. In 2018, the annual count of 1,801,010 visits for mental health disorders represented a decrease of 5.8% from 2014 and a 7.3% decrease from 2016. Three major illness- and injury-related categories (musculoskeletal system/connective tissue disorders, disorders of the nervous system and sense organs, and respiratory system disorders) showed increased numbers of visits and rates in 2018 compared to 2014. Except as described, the annual numbers of visits and the rates for most (14 of 17) of the major diagnostic categories have recently declined. This downward trend is likely due, in part, to the ongoing drawdown of military forces; for example, at the end of Sept. 2018, there were approximately 21,000 fewer active duty military personnel than at the same time in 2014.2
During 2014–2018, the relative ranking of injury/poisoning (rank: 6) as a primary cause of ambulatory visits has been stable. However, the numbers and rates of visits for injury/poisoning have declined by 8.6% and 5.6%, respectively, since 2014. Nevertheless, the potential military operational impacts of various conditions cannot be assessed by numbers of attributable ambulatory visits alone. For example, in 2018, injuries and poisonings accounted for approximately 1 of every 22 ambulatory visits overall; however, of ambulatory visits occurring at MTFs, 17.9% (slightly more than 1 in 6) had limited duty dispositions. Of particular note, in relation to injuries and musculoskeletal conditions, in 2018 (as in the past), joint and back injuries and other disorders accounted for large numbers of ambulatory visits; resources should continue to be focused on preventing, treating, and rehabilitating back pain and injuries among active component members.
It should be noted that the summary data using the major diagnostic categories of the ICD-10 system presented here deserve as detailed an examination as presented in Tables 2 and 3. For example, the general category identified as "nervous system" encompasses diseases of the nervous system and the sense organs (eyes and ears). Results presented in Tables 2 and 3 indicate that the more common diagnoses in this category refer to sleep disorders, disorders of refraction and accommodation, and pain disorders. Closer scrutiny reveals that the overall increase (n=200,167) in annual visits for this category from 2014 to 2018 (described earlier) can be attributed mostly to a rise in diagnoses of organic sleep disorders from 359,675 in 2014 to 502,446 in 2018.3
Several limitations should be considered when interpreting the findings of this report. For example, ambulatory care that is delivered by unit medics and at deployed medical treatment facilities (such as in Afghanistan or Iraq or at sea) may not be documented on standardized, automated records and thus not archived in the DMSS. In turn, this summary does not reflect the experience of active component military members overall, to the extent that the natures and rates of illnesses and injuries may vary between those who are deployed and those who are not deployed.
In addition, this summary is based on primary (first-listed) diagnosis codes reported on ambulatory visit records. As a result, the current summary discounts morbidity related to comorbid and complicating conditions that may have been documented in secondary diagnostic positions of the health care records. Furthermore, the accuracy of reported diagnoses likely varies across conditions, care providers, treatment facilities, and clinical settings. Although some specific diagnoses made during individual encounters may not be definitive, final, or even correct, summaries of the frequencies, natures, and trends of ambulatory encounters among active component members are informative and potentially useful. For example, the relatively large numbers of ambulatory visits for mental health disorders in general and the large numbers of visits for organic sleep disorders among males reflect patterns of responses by the MHS to the effects of combat- and deployment-related stresses on active component service members.
Also, this report documents all ambulatory health care visits but does not provide estimates of the incidence rates of the diagnoses described. In contrast to common, self-limited, and minor illnesses and injuries that require very little, if any, follow-up or continuing care, illnesses and injuries that necessitate multiple ambulatory visits for evaluation, treatment, and rehabilitation are overrepresented in this summary of the ambulatory burden of health care. Finally, the new electronic health record, MHS GENESIS, was implemented at several MTFs during 2017. Medical data from sites using MHS GENESIS are not available in the DMSS. These sites include Naval Hospital Oak Harbor, Naval Hospital Bremerton, Air Force Medical Services Fairchild, and Madigan Army Medical Center. Therefore, medical encounter data for individuals who received outpatient care at any of these facilities during 2018 were not included in this analysis.
References
- Armed Forces Health Surveillance Branch. Ambulatory visits, active component, U.S. Armed Forces, 2016. MSMR. 2017;24(4):16–22.
- Defense Manpower Data Center. DOD personnel, workforce reports and publications. Active duty military personnel by service by rank/grade. Sept. 2018 and FY 2014. https://www.dmdc.osd.mil/appj/dwp/dwp_reports.jsp. Accessed April 11, 2019.
- Armed Forces Health Surveillance Center. Ambulatory visits among members of the active component, U.S. Armed Forces, 2014. MSMR. 2015;22(4):18–24.