What Are the New Findings?
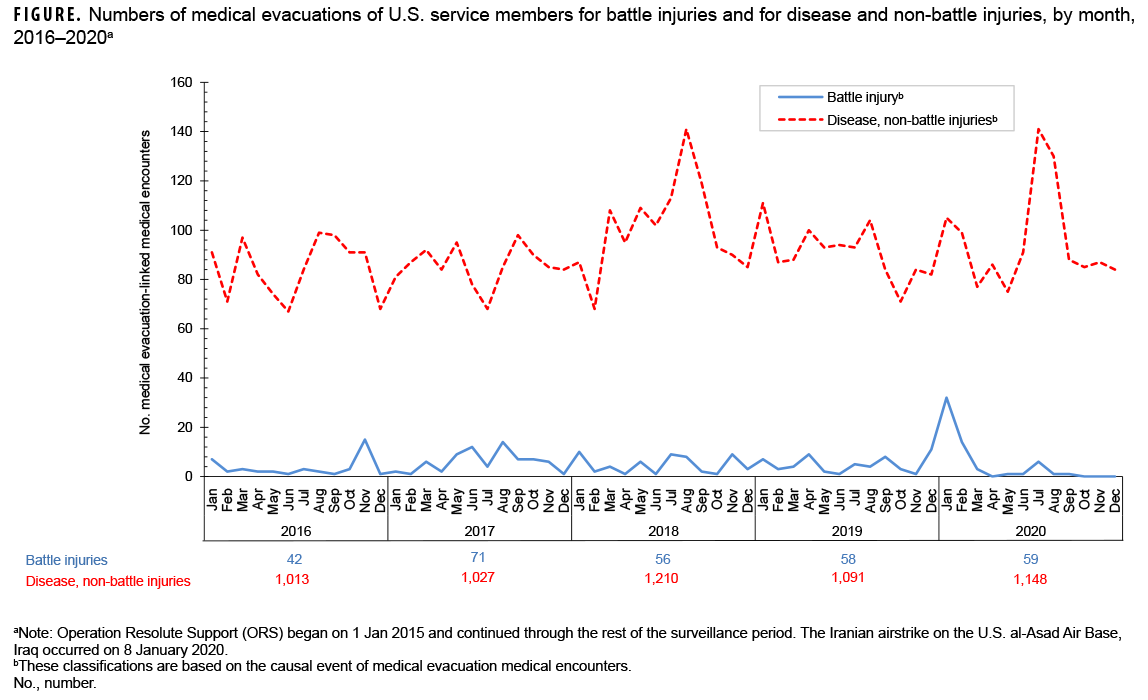
The numbers of medical evacuations of service members in 2020 were roughly similar to the numbers for the previous 4 years. The proportions of evacuations that were due to battle injuries remained relatively steady during this period except for a small peak in January 2020. Evacuations for mental health disorders were the most common, followed by non-battle injury and poisoning, and COVID-19.
What Is the Impact on Readiness and Force Health Protection?
Only 1,207 service members were evacuated during 2020, but the process of medical evacuation of service members to Europe and CONUS is logistically demanding. The effort expended to evacuate service members to sources of definitive, modern health care is a reassuring investment in the health, welfare, and importance of the men and women serving overseas.
Background
Although there have been substantial reductions in combat operations taking place in the U.S. Central Command (CENTCOM) area of responsibility (AOR) in Southwest Asia,1 the number of service members deployed to the CENTCOM AOR is still significant. Recent reports indicate that there are about 60–80,000 U.S. troops in the CENTCOM AOR.2,3 In theaters of operations such as Afghanistan, most medical care is provided by deployed military medical personnel; however, some injuries and illnesses require medical management outside the operational theater. In these cases, the affected individuals are usually transported by air to a fixed military medical facility in Europe or the U.S. where the service members receive the specialized, technically advanced, and/ or prolonged diagnostic, therapeutic, and rehabilitative care required.
The ongoing pandemic of coronavirus disease 2019 (COVID-19) has presented additional challenges to readiness for service members stationed in CENTCOM. According to the May 2020 U.S. CENTCOM COVID-19 Pandemic Playbook for Operational Environments, all persons who test positive for COVID-19 are recommended to be moved into isolation and prepared for evacuation out of theater.4 A prior MSMR report identified 186 air evacuations for COVID-19 originating from CENTCOM through the end of September 2020, which included positive cases and close contacts.5
Medical air transports, or medical evacuations, are costly and generally indicative of serious medical conditions. Some serious conditions are directly related to participation in or support of combat operations (e.g., battle wounds); however, many other conditions are unrelated to combat and may be preventable. This report summarizes the natures, numbers, and trends of conditions for which male and female military members were medically evacuated from CENTCOM AOR operations during 2020 and compares them to the previous 4 years.
Methods
The surveillance period was 1 Jan. 2016 through 31 Dec. 2020. The surveillance population included all members of the active and reserve components of the U.S. Army, Navy, Air Force, and Marine Corps who were deployed to the CENTCOM AOR during the period. The outcome of interest in this analysis was medical evacuations during the surveillance period from the CENTCOM AOR (e.g., Afghanistan or Iraq) to a medical treatment facility outside the CENTCOM AOR. Records of all medical evacuations conducted by the U.S. Transportation Command (TRANSCOM) maintained in the TRANSCOM Regulating and Command & Control Evacuation System (TRAC2ES) were utilized. Evacuations were included in the analysis if the affected service member had at least 1 inpatient or outpatient medical encounter in a permanent military medical facility in the U.S. or Europe during a time interval extending from 5 days before to 10 days after the reported evacuation date.
Medical evacuations included in the analyses were classified by the causes and natures of the precipitating medical conditions (based on information reported in relevant evacuation and medical encounter records). First, all medical conditions that resulted in evacuations were classified as either "battle injuries" or "non-battle injuries and illnesses"(based on entries in an indicator field of the TRAC2ES evacuation record). Evacuations due to non-battle injuries and illnesses were subclassified into 17 illness/injury categories based on International Classification of Diseases, 9th and 10th Revisions (ICD-9 and ICD-10, respectively) diagnostic codes reported on the records of medical encounters after evacuation. In addition, a new category was added this year for evacuations that resulted in a diagnosis of COVID-19 (ICD-10: U07.1). For the purposes of this report, all records of hospitalizations and ambulatory visits from 5 days before to 10 days after the reported date of each medical evacuation were identified. In most cases, the primary (first-listed) diagnosis for either a hospitalization (if any occurred) or the earliest ambulatory visit after evacuation was considered indicative of the condition responsible for the evacuation. However, if the first-listed diagnostic code specified the external cause (rather than the nature) of an injury (ICD-9 E-code/ICD-10 V-, W-, X-, or Y-code) or an encounter for something other than a current illness or injury (e.g., observation, medical examination, or vaccination [ICD-9 V-codes/ICD-10 Z-codes other than those related to pregnancy]), then secondary diagnoses that specified illnesses and injuries (ICD-9: 001– 999/ICD-10: A00–T88) were considered the likely reasons for the subject evacuations. If there was no secondary diagnosis or if the secondary diagnosis also was an external cause code, the first-listed diagnostic code of a subsequent encounter was used. To better understand the reasons for medical evacuations among those whose only diagnoses post-evacuation were for administrative examinations, the patients' histories documented in the TRAC2ES records were examined.
The disposition after each medical evacuation was determined by using the disposition code associated with the medical encounter that was used for documenting the category of the medical evacuation. Inpatient disposition categories were returned to duty (code 01), transferred/discharged to other facility (codes 02–04, 09, 21–28, 43, or 61–66), died (codes 20, 30, 40–42, 50, or 51), separated from service (codes 10–15), and other/unknown. Outpatient disposition categories were released without limitation (code 1), released with work/duty limitation (code 2), immediate referral (code 4), sick at home/quarters (codes 3 or S), admitted/ transferred to civilian hospital (codes 7, 9, A–D, or U), died (codes 8 or G), discharged home (code F), and other/unknown.
Results
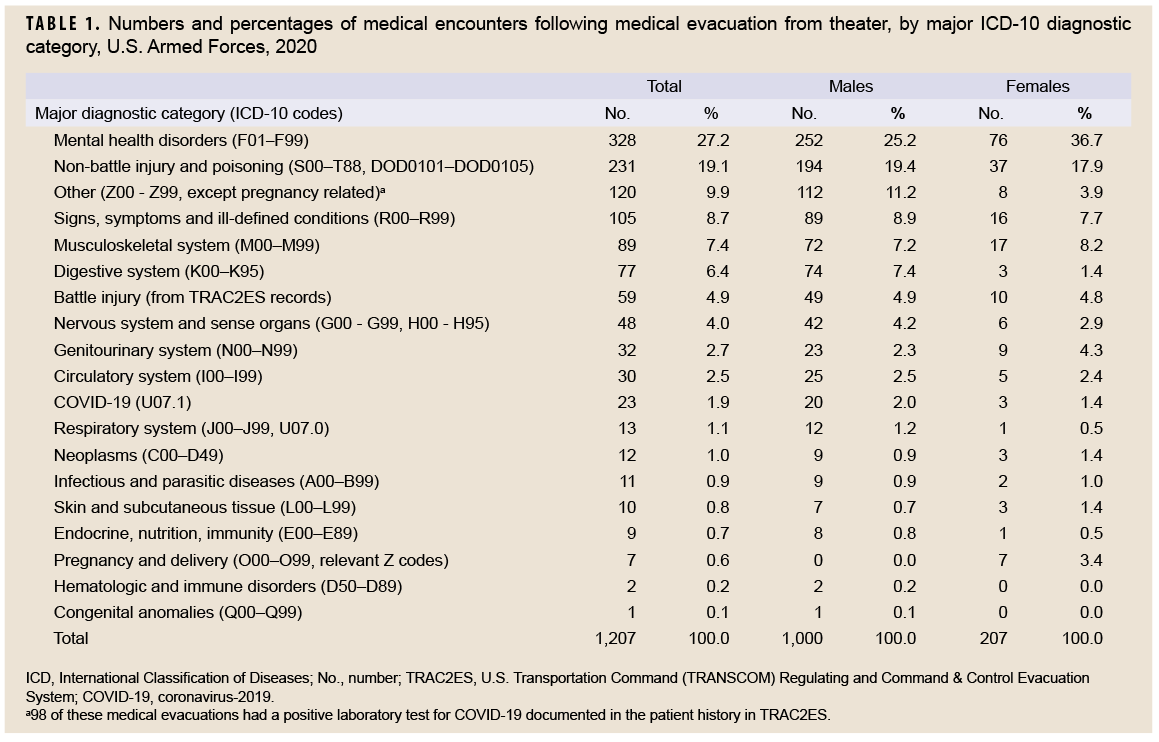
In 2020, a total of 1,207 medical evacuations of service members from the CENTCOM AOR were followed by at least 1 medical encounter in a fixed medical facility outside the operational theater (Table 1). Overall, there were more medical evacuations for mental health disorders (n=328; 27.2%) than for any other single category of illnesses or injuries. In order of decreasing frequency, the categories with the next most common medical evacuations were non-battle injuries and poisonings (n=231; 19.1%); other conditions (ICD-10: Z00-Z99, except pregnancy-related codes; n=120; 9.9%); signs, symptoms, and ill-defined conditions (n=105; 8.7%); musculoskeletal system/connective tissue disorders (n=89; 7.4%); and disorders of the digestive system (n=77; 6.4%). All of the above categories were associated with more evacuations than the number of evacuations for battle injuries (n=59; 4.9%). The top 3 categories—mental health disorders (most frequently adjustment and depressive disorders); non-battle injuries (primarily fractures of extremities, strains, and sprains); and other conditions (primarily encounters for administrative examinations)—accounted for more than half (56.3%) of all evacuations (Table 1). Upon examination of the patient history documented in the TRAC2ES record, 99 of the 120 evacuations for other conditions mentioned COVID-19 as the primary indication for medical evacuation and almost all of these records (n=98) also mentioned the patient having a positive laboratory test result for COVID-19 (data not shown).
During 2016–2020, the annual number of medical evacuations attributable to battle injuries was highest in 2017 (n=71), decreased in 2018 (n=56), and remained relatively stable through 2019 (n=58) and 2020 (n=59) (Figure). However, there was a peak in the monthly number of medical evacuations attributable to battle injuries in January 2020 (n=32) (Figure). The annual number of medical evacuations attributable to non-battle injuries and diseases remained relatively stable, ranging between a low level in 2016 (n=1,013) and a peak in 2018 (n=1,210). The number in 2020 (n=1,148) was the second highest count during the 5-year period.
Demographic and military characteristics.
The number of medical evacuations in 2020 was higher among males (n=1,000) than females (n=207) (Table 1, 2). The most frequent causes of medical evacuations among male service members were mental health disorders (n=252; 25.2%); non-battle injury and poisoning (n=194; 19.4%); other conditions (n=112; 11.2%); and signs, symptoms, and ill-defined conditions (n=89; 8.9%) (Table 1). Among female service members, the most frequent causes of medical evacuations were mental health disorders (n=76; 36.7%); non-battle injury and poisoning (n=37; 17.9%); musculoskeletal system conditions (n=17; 8.2%); and signs, symptoms, and ill-defined conditions (n=16; 7.7%).
Compared to males, female service members had notably higher percentages of medical evacuations for mental health disorders and genitourinary system disorders (Table 1). In contrast, male service members had higher percentages of evacuation for non-battle related injuries, other conditions (encounters for administrative examinations for COVID-19), and digestive system conditions.
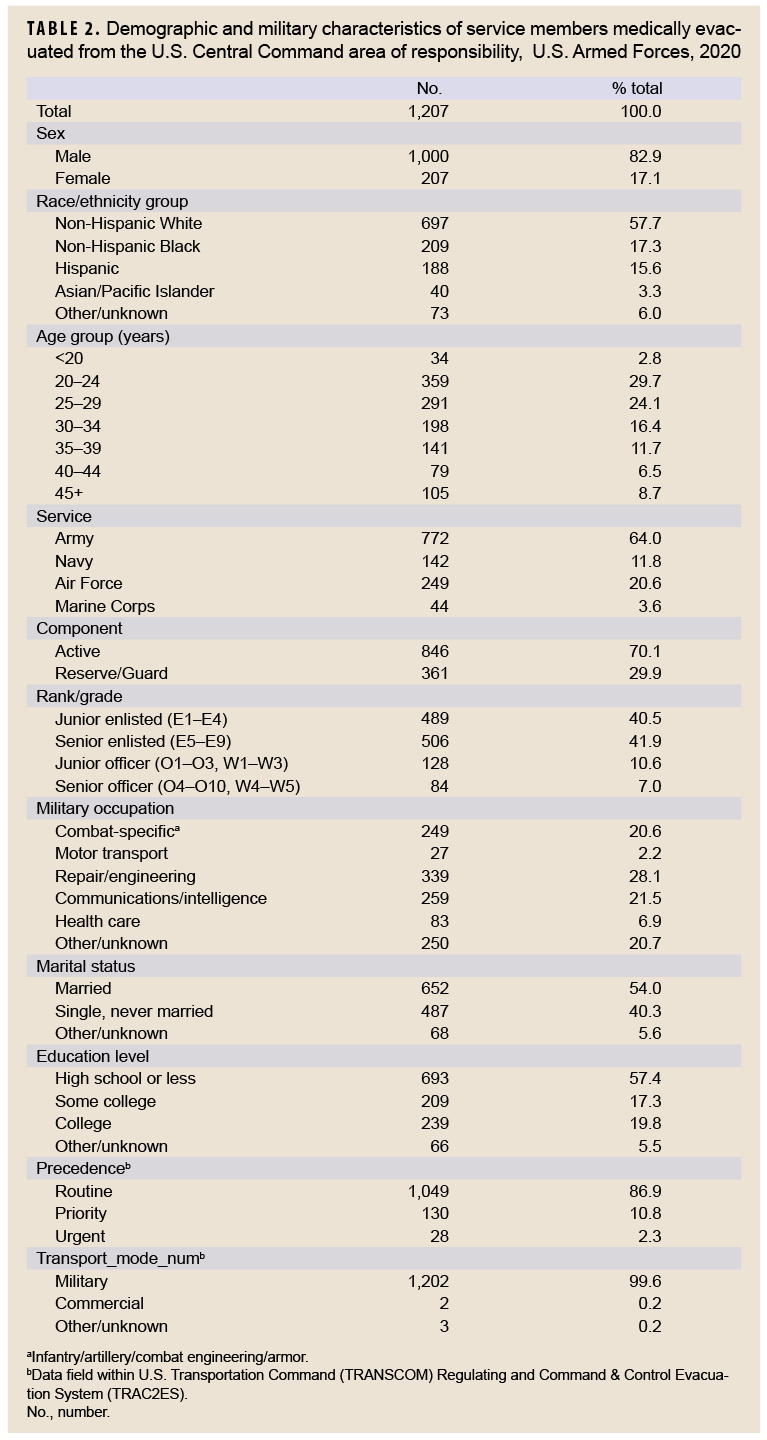
Within the various demographic and military characteristics of those service members who were evacuated, the largest numbers and proportions of evacuees were among non-Hispanic White service members, those aged 20–24 years, members of the Army, junior and senior enlisted personnel, and those in repair/engineering occupations (Table 2). In 2020, most medical evacuations (86.9%) were characterized as having routine precedence. The remainder had priority (10.8%) or urgent (2.3%) precedence. All but 5 (0.4%) of the medical evacuations were accomplished through military transport (Table 2).
Most frequent specific diagnoses
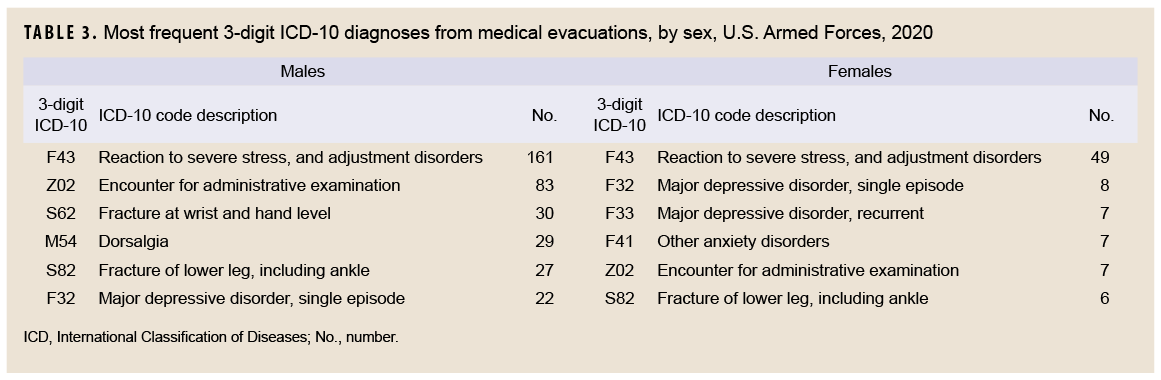
Among both males and females in 2020, a mental health disorder ("reaction to severe stress, and adjustment disorders") was the most frequent specific diagnosis (3-digit ICD-10 diagnosis code: F43) during initial medical encounters after evacuations (Table 3). The second most common 3-digit diagnosis for males, and the fifth most common for females, was Z02 ("encounter for administrative examination"). The next most common 3-digit diagnoses for males were fractures at the hand and wrist level, dorsalgia, fracture of the lower leg, and major depressive disorder. For females, the second through fourth most common 3-digit diagnoses were for major depressive disorders (single episode and recurrent), and other anxiety disorders (Table 3).
Disposition
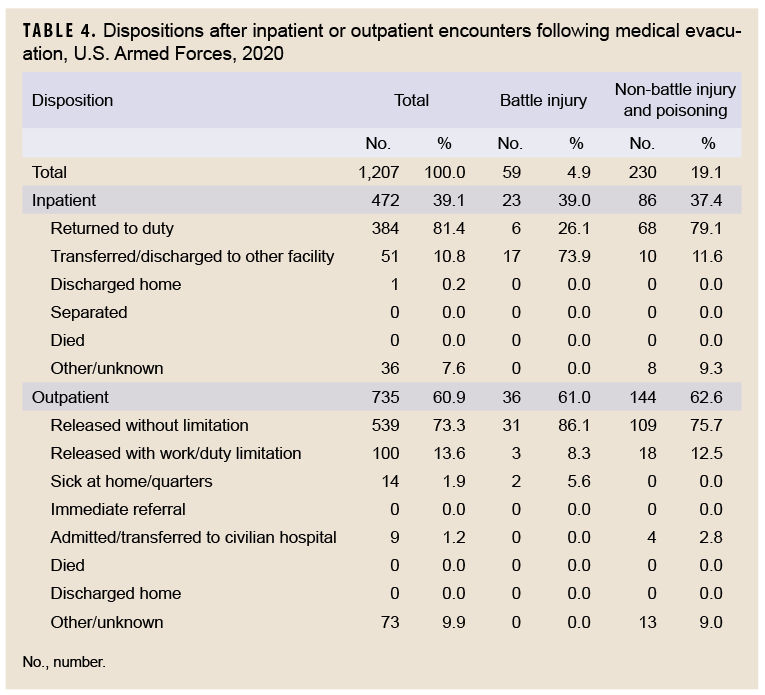
Of the 1,207 medical evacuations reported in 2020, a total of 472 (39.1%) resulted in inpatient encounters. About four-fifths (81.4%) of all service members who were hospitalized after medical evacuations were discharged back to duty. Slightly more than one-tenth (10.8%) of service members who were hospitalized after medical evacuations were transferred or discharged to other facilities (Table 4).
Return to duty dispositions were much more likely after hospitalizations for nonbattle injuries (79.1%) than for battle injuries (26.1%). The majority (73.9%) of battle injury-related hospitalizations and a little more than one-tenth (11.6%) of non-battle injury-related hospitalizations resulted in transfers/discharges to other facilities (Table 4).
About three-fifths (n=735; 60.9%) of all medical evacuations resulted in outpatient encounters only. Of the service members who were treated exclusively in outpatient settings after evacuations, the majority (73.3%) were discharged back to duty without work/duty limitations; 13.6% were released with work/duty limitations; 1.9% were discharged to "home sick" for recuperation; and 1.2% were admitted/transferred to a civilian hospital. Service members treated as outpatients after battle injury-related evacuations were more likely to be released without limitations (n=31; 86.1%) than medical evacuees treated as outpatients for non-battle injuries (n=109; 75.7%) (Table 4).
Editorial Comment
This report documented that only 4.9% of all medical evacuations during 2020 were associated with battle injuries. Counts of evacuations for battle injuries remained relatively low during the surveillance period, likely reflecting the reduced amount of combat operations in the CENTCOM AOR as compared to the prior years of Operation Iraqi Freedom and Operation Enduring Freedom. However, there was a small spike in the number of medical evacuations for battle injuries in January 2020. Several of these evacuations appeared to be related to the Iranian ballistic missile attack on the U.S. al-Asad Air Base in Iraq.6
Most evacuations in 2020 were attributed to mental health disorders, followed by non-battle injuries and poisonings; administrative examinations for COVID19; signs, symptoms, and ill-defined conditions; and musculoskeletal disorders. Evacuations during the entire 5-year surveillance period followed a similar but slightly different pattern, with mental health disorders being the most frequent followed by non-battle injuries; signs, symptoms and ill-defined conditions; musculoskeletal disorders; and digestive system disorders. In 2020, male service members had higher percentages of evacuation for non-battle related injuries, other conditions (encounters for administrative examinations for COVID-19), and digestive system conditions compared to female service members. As in previous years, the majority of service members who were evacuated were returned to normal duty status following their post-evacuation hospitalizations or outpatient encounters. In addition, 63% of those evacuated for battle injuries were returned to duty immediately after their initial health care encounters.
Overall, the changes in numbers of medical evacuations over the course of the surveillance period reflect the end of Operation Enduring Freedom in 2014, the beginning of Operation Freedom's Sentinel, and the deployment of troops to Afghanistan, Iraq, and Syria.3 The relatively low percentage of medical evacuations in 2020 suggests that most deployers were sufficiently healthy and ready for their deployments and received the medical care in theater necessary to complete their assignments without having to be evacuated. Moreover, the fact that very few medical evacuations were conducted for chronic conditions such as hematologic disorders and congenital anomalies supports the idea that most deployers were sufficiently healthy for deployment. However, it is not surprising that such conditions are occasionally diagnosed among deployed service members. For example, there was 1 medical evacuation for congenital anomalies in 2020 that was due to Meckel's diverticulum, a bulge in the lower part of the small intestine that is leftover from the umbilical cord at birth (data not shown). Because congenital anomalies may not be identified and diagnosed until later in life,7 the infrequent detection of such diagnoses during deployment is not unexpected.
The proportion of medical evacuations attributed to mental health disorders (27.2%) was very similar to the proportion reported in recent MSMR analyses of medical evacuations in 2019 (27.1%) and considerably higher than the proportion (11.6%) reported in an earlier MSMR report examining evacuations from Iraq during a 9-year period between 2003 and 2011.1,8 However, that article also reported that during the last 4 years of the surveillance period (2008–2011), as the proportion of evacuations for battle injuries fell sharply, the proportions of evacuations for mental health disorders increased dramatically for both males (peak of 20.9% in 2010) and females (peak of 26.6% in 2010). Although some studies have indicated improved access to mental health care in deployed settings, the results from the current analysis indicate that mental health diagnoses still represent the single most common basis for medical evacuations out of the CENTCOM AOR.9 This could be due, at least in part, to variations in the availability of mental health care in deployed settings. In these settings, the distribution of providers and clinics that deliver such services is uneven and varies according to factors such as the number of deployed personnel and the assessed needs of the particular unit.9 In addition, although the number of mental health care providers in Afghanistan increased from 2005 through 2010, this number decreased after 2013 as part of the overall drawdown of U.S. troops from the region.9
COVID-19 accounted for a significant number of medical evacuations out of CENTOM AOR in 2020. However, many of these evacuations were documented as administrative examinations. If the total number of evacuations for administrative examinations that also documented a positive laboratory test result for COVID-19 in the TRAC2ES patient history field (n=98) are considered, then the total number of evacuations for COVID-19 would be 121, which is much higher than the 23 records that had a diagnosis for U07.1. Taking into account these administrative examinations would make COVID-19 the third leading cause of medical evacuation out of CENTCOM AOR in 2020. However, not all of these evacuations may have been medically necessary and may have instead been driven by guidance, policies, and procedures in-theater.4,5
Several important limitations should be considered when interpreting the results of this analysis. Direct comparisons of numbers and percentages of medical evacuations by cause, as between males and females, can be misleading; for example, such comparisons do not account for differences between the groups in other characteristics (e.g., age, grade, military occupation, locations, and activities while deployed) that are significant determinants of medical evacuation risk. Moreover, because data about the characteristics of the entire deployed population of service members were not available, it was not possible to determine if the members of demographic and military groups listed above were over- or underrepresented among the evacuees. Also, for this report, most causes of medical evacuations were estimated from primary (first-listed) diagnoses that were recorded during hospitalizations or initial outpatient encounters after evacuation. In some cases, clinical evaluations in fixed medical treatment facilities after medical evacuations may have ruled out serious conditions that were clinically suspected in theater. For this analysis, the causes of such evacuations reflect diagnoses that were determined after evaluations outside of the theater rather than diagnoses—perhaps of severe disease—that were clinically suspected in theater. To the extent that this occurred, the causes of some medical evacuations may seem surprisingly minor.
Overall, the results highlight the continued need to tailor force health protection policies, training, supplies, equipment, and practices based on characteristics of the deployed force (e.g., combat vs. support; male vs. female) and the nature of the military operations (e.g., combat vs. humanitarian assistance).
References
- Armed Forces Health Surveillance Branch. Medical evacuations out of the U.S. Central Command, active and reserve components, U.S. Armed Forces, 2019. MSMR. 2020;27(5):27–32.
- McInnis, KJ. The 2019-2020 Iran Crisis and U.S. Military Deployments. Congressional Research Service. 9 January 2020. Accessed 11 April 2021.
- Lead Inspector General for Overseas Contingency Operations. Operation Freedom’s Sentinel: Report to the United States Congress. Accessed 11 April 2021. https://www.stateoig.gov/system/ files/lead_inspector_general_for_operation_freedoms_sentinel_dec_2020.pdf.
- U.S. Central Command. COVID-19 Pandemic Playbook for Operational Environments. 12 May 2020. Accessed 25 March 2021. https://jts.amedd.army.mil/assets/docs/USCENTCOM_COVID-19_ Pandemic_Playbook.pdf
- Stanila V, Wells N, Ziadeh C, Stahlman S. Air Evacuation of Service Members for COVID-19 in U.S. Central Command and U.S. European Command From 11 March 2020 Through 30 September 2020. MSMR. 2020;27(12):14–17.
- Correll, DS and Snow S. Eleven Troops Injured after Iran’s Strike against al-Asad Airbase, says CENTCOM. Military Times. January 17, 2020. Accessed 07 May 2021.
- The Centers for Medicare and Medicaid Services and the National Center for Health Statistics. ICD-10-CM Official Guidelines for Coding and Reporting. FY 2021. Accessed 11 April 2021. https:// www.cdc.gov/nchs/data/icd/10cmguidelinesFY2021.pdf
- Armed Forces Health Surveillance Center. Medical evacuations from Operation Iraqi Freedom/Operation New Dawn, active and reserve components, U.S. Armed Forces, 2003–2011. MSMR. 2012;19(2):18–21.
- United States Government Accountability Office. Report to Congressional Committees. Defense health care: DOD is meeting most mental health care access standards, but it needs a standard for follow-up appointments. April 2016. Accessed 11 April 2021. https://www.gao.gov/assets/680/676851.pdf