Mental Health Panel Discusses Impact of COVID-19
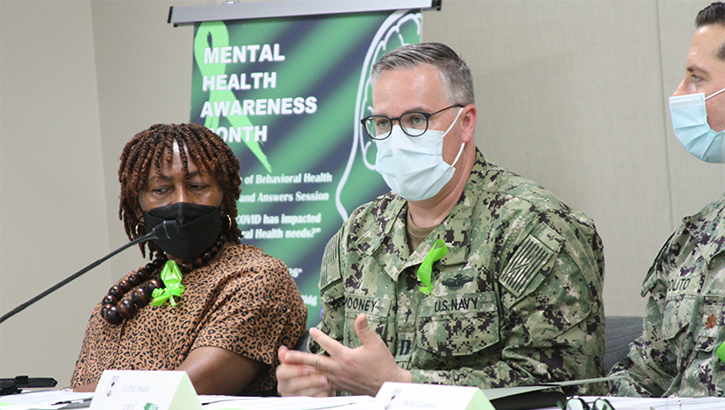 Navy Chaplain (Lt.) Kevin Mooney said, “It is a sign of strength and it is a sign of wisdom,” for people to seek behavioral health services when in need. “If you sprain your knee or you have a cut, you take care of it. When we have struggles internally, invisible wounds, it just makes sense to seek help,” he explained during a panel presentation at Walter Reed National Military Medical Center May 26 (Photo by: Bernard S. Little, Walter Reed National Military Medical Center).
Navy Chaplain (Lt.) Kevin Mooney said, “It is a sign of strength and it is a sign of wisdom,” for people to seek behavioral health services when in need. “If you sprain your knee or you have a cut, you take care of it. When we have struggles internally, invisible wounds, it just makes sense to seek help,” he explained during a panel presentation at Walter Reed National Military Medical Center May 26 (Photo by: Bernard S. Little, Walter Reed National Military Medical Center).
"How has COVID-19 impacted behavioral health needs?"
This was the question discussed during the Directorate of Behavioral Health's Mental Health Panel session on May 26 at Walter Reed National Military Medical Center (WRNMMC) in Bethesda, Maryland.
Panel members included health-care providers, spiritual leaders and support services personnel from throughout the WRNMMC community. All agreed that the year and a half people have faced the COVID-19 pandemic has been challenging on multiple fronts, affecting the mental health of many individuals.
"The Mental Health Awareness Panel affords beneficiaries and clinicians the opportunities to generate discussions on how Behavioral Health [services] have addressed the increase in mental health concerns across Tricare beneficiaries during the pandemic," Army Maj. Darlene Lazard explained. Lazard, deputy director for Behavioral Health at WRNMMC, coordinated the event.
"Unfortunately, we have had an increase in sexual assault reporting, and an increase in sexual harassment concerns [since the pandemic began]," said Evarlean Rumph, command sexual assault response coordinator at WRNMMC. Behavioral health providers state extreme stress, uncertainties because of job loss, reduced working hours and other concerns, fear, quarantine, social isolations and movement restrictions, all have raised concern for increases in assault and abuse.
"Mental health services are always offered during our intake briefing to all of our clients. [Many] feel mental health services add a positive impact on their healing process," Rumph said.
Navy Lt. Cmdr. Michael Polito, a child and adolescent psychologist at WRNMMC, said similar to other services at the medical center, his department has seen "a trend in flux of needs" among beneficiaries. "We usually see a lot of acute cases within our service, but there's been much more of a stress on families as they hunkered down together and tried to navigate the world of virtual learning.
He also noted virtual learning came with stressors because schools weren't prepared for it and there were hiccups. Families had to deal with time management issues, and in some cases, kids' grades dropped because of the change from in-person learning.
"A lot of the services we focused on was providing problem-solving solutions," Polito continued. "We sort of shifted our treatment modalities to what's the problem and how we solve it, versus [previously] focusing more on pathology."
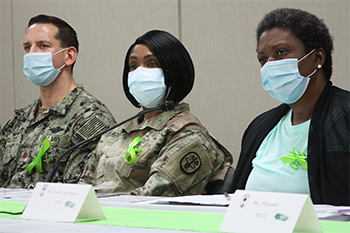 A panel of behavioral and spiritual health providers discuss how COVID-19 has impacted behavioral health needs during a presentation May 26 at Walter Reed National Military Medical Center (Photo by: Bernard S. Little, Walter Reed National Military Medical Center).
A panel of behavioral and spiritual health providers discuss how COVID-19 has impacted behavioral health needs during a presentation May 26 at Walter Reed National Military Medical Center (Photo by: Bernard S. Little, Walter Reed National Military Medical Center).
Polito added the virtual platform has also had its advantages. "It's been a real helpful way to access care for our beneficiaries," he said.
Lisa Turner-McDougald, the parent support home visitor with Fleet and Family at Fort Meade, Maryland, said she also saw an increase of stress among families caused by virtual learning during the pandemic. "It's hard [for kids] to sit in front of a computer all day long when that was not their learning style or something they're used to doing," she explained. She added she assisted families with webinars she offered which focused on time management and tapping into the various learning styles of children to help them adjust.
Turner-McDougald said she also recommended to parents and caregivers to have Zoom parties and game nights so children did not feel too isolated during the pandemic.
Navy Chaplain (Lt.) Kevin Mooney said when the pandemic began, he was at another command. "I struggled the first 90 days because we were restricted to a 50-miles radius. At Camp Lejeune, North Carolina, there's nothing within 50 miles. So some days were better than others." He added he and some friends would bike ride on some days, which helped with the feeling of isolation.
The panelists agreed that reaching out to family, friends and in some cases, colleagues, can be beneficial in dealing with stress. They also recommend taking quiet time to yourself to relax and de-stress, as well as exercising.
"We're set up to support one another," said Tonya Pleasant, a military family life counselor at WRNMMC. "Something that's real important to me is self-care, and practicing what I preach. If I'm encouraging a service member to do different things, eating right, getting sunshine and other coping strategies, I would definitely be remiss in not doing that myself."
In addition to the stress of the pandemic, panel members addressed the anxiety caused by various social and political issues taking place in the United States.
"I was sort of struck by just how young the kids who I saw were who were reporting their concerns with issues regarding racial justice," Polito said. "[The issue] is something that is certainly impacting a broad swath of children and adolescents across demographics. I think it was helpful for the community of children and adolescent psychiatry and psychology in challenging us regarding how we address those issues in making sure we're providing culturally sensitive intervention in addressing the concerns of our patients. It was a growing experience for our therapeutic interventions.
The panelists also agreed it's not a sign of weakness to seek help for behavioral health concerns. "We all have pretty much something going on in our lives," Lazard said. "It's a sign of strength knowing that you may need these services," Turner-McDougald added. "It's not a stigma any longer to seek help."
"It is a sign of strength and it is a sign of wisdom," Mooney furthered. "If you sprain your knee or you have a cut, you take care of it. When we have struggles internally, invisible wounds, it just makes sense to seek help."
According to the National Institutes of Health's National Institute of Mental Health (NIMH), mental health impacts of COVID-19 will outlive the pandemic itself. NIMH states it's crucial for people and agencies to work together to apply evidence-based strategies to support the mental health needs of all Americans and to make these strategies broadly available, especially in vulnerable communities.
The WRNMMC sexual assault victim hotline is available 24/7 at 301-442-8225. The SARC is available 24/7 at 301-442-2053. The DoD Safe Helpline is 1-877-995-5247.