Background
Since the official introduction of laser refractive surgery into clinical practice throughout the Military Health System (MHS) in fiscal year 2000, these techniques have been heavily implemented in the tri-service community to better equip and improve the readiness of the U.S. military force. Military studies of refractive surgery date back to 1993, but prior to full military utilization of laser refractive surgery, spectacles or contact lenses were the mainstay to correct refractive error among military personnel.1,2 Studies on the prevalence of refractive error, including myopia, hyperopia, and astigmatism, have shown that these conditions are quite common among active component service members.3,4 Reversing such error through refractive surgery has been documented to improve military readiness, operational capability, and the quality of life of U.S. service members.5
There are 26 Department of Defense (DOD) Warfighter Refractive Surgery Centers that offer a combination of vision-correcting procedures such as photorefractive keratectomy (PRK), laser assisted in situ keratomileusis (LASIK), laser epithelial keratomileusis (LASEK), small incision lenticule extraction (SMILE), implantable collamer lens (ICL), and refractive lens exchange (RLE).6–8 The capability to readily perform surgery with laser technology using the latest refractive surgery platforms highlights the importance of optimized vision to the DOD.
The COVID-19 pandemic introduced numerous obstacles which contributed to the reduction in the number of procedures performed. These obstacles included the closure of surgical centers and lack of temporary duty travel (TDY) patients. The pandemic also resulted in a shift to pre-operative testing for COVID-19 and virtual pre-operative briefings which could potentially result in delayed or cancelled refractive surgeries.
The objective of this report was to describe trends in total numbers of refractive surgeries over the last 21 fiscal years and to demonstrate how the early COVID-19 pandemic affected military refractive surgery trends.
Methods
Data on all refractive surgery cases performed at 26 DOD Warfighter Refractive Surgery Centers were compiled by the U.S. Navy refractive surgery program manager and presented at the 2021 virtual Military Refractive Surgery Safety and Standards Symposium annual meeting.6–8 These data are summarized in this report.
The surveillance period was from 1 Oct. 1999 through 30 Sept. 2020 (fiscal years 2000–2020). The surveillance population included active duty service members (active component and activated Reserve/Guard members) who met eligibility criteria for refractive eye surgery. Criteria for qualifying for refractive surgery may have differed among the services, but in general, service members had to have had at least 18 months left in their service commitments, a commander's authorization letter, and no adverse personnel actions. In addition, 3 Air Force locations performed refractive surgery on a small number of non-service member beneficiaries of the Military Health System as part of a research protocol (accounting for <0.03% of Air Force refractive surgical cases for fiscal year 2020).
Results
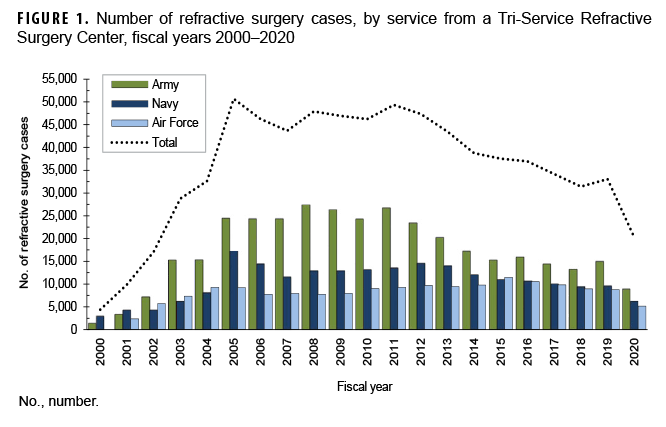
For fiscal years 2000–2020, a total of 746,950 refractive surgeries were reported from the 26 Warfighter Tri-Service Refractive Surgery Centers. The number of surgeries performed each fiscal year ranged from a low of 4,381 refractive surgeries in 2000 to a peak of 50,690 surgeries in 2005 (Figure 1) with an average of 35,569 surgeries per year. In fiscal year 2020, 20,270 refractive surgeries were performed which represents a 38.6% decrease from the number of cases performed in 2019 (n=33,039).
During the surveillance period, there were 363,058 surgeries performed at Army refractive centers, 216,568 at Navy refractive centers, and 167,324 at Air Force refractive centers. The number of surgeries for all services declined from fiscal year 2019 to fiscal year 2020 (Army, 39.8% decrease; Navy, 34.6% decrease; Air Force, 41.0% decrease) (Figure 1).
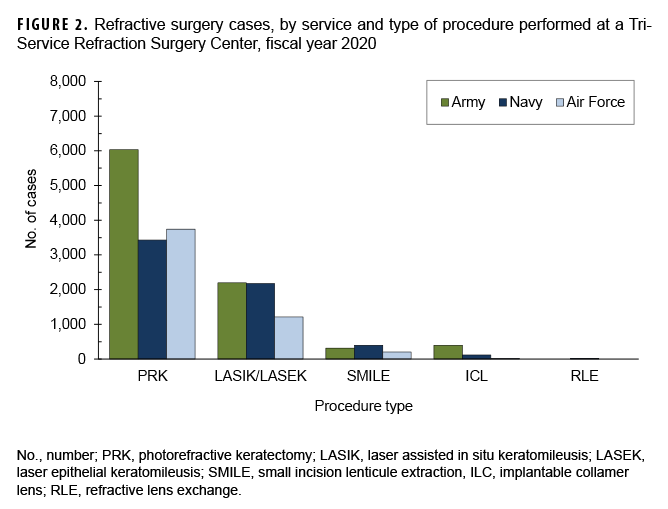
In 2020, the types of refractive surgery approximately consisted of 65.1% PRK (n=13,201), 27.6% LASIK/LASEK (n=5,585), 4.5% SMILE (n=920), 2.7% ICL (n=540), and 0.1% RLE (n=24) (Figure 2). The percentage distributions of type of refractive surgery were similar among all the services in 2020.
Editorial Comment
This report describes trends in the numbers of refractive surgeries performed during the 21 year surveillance period, including the COVID-19 pandemic. Since fiscal year 2000, the tri-service ophthalmology community conducted 746,950 vision corrective surgeries at 26 DOD Warfighter Refractive Surgery Centers. The large number of refractive cases reported and the amount of refractive surgery centers present in the DOD speaks to the valued importance of optimal vision in U.S. military members. In addition to the warfighter's improvement in quality of life, vision corrective surgeries are used frequently in the U.S. military due to the need and for improved preparedness and performance in operational tasks.3–5 An Air Force study from 2020 reported the prevalence of myopia in 767 Air Force Basic Military Trainees. Among the trainees, 45% were found to have myopia classified as greater than -0.5 D, and 2% of trainees were found to have high myopia classified as greater than -6.0 D.4 In 2019, Reynolds et al. reported that 51.1% of ocular care for service members during fiscal year 2018 was dedicated to refractive error-related disorders.9 A study published in 2017 demonstrated the excellent and comparable vision outcomes of Wave-Front Guided and Wave-Front Optimized PRK on military members in regard to marksmanship, visual performance, threshold target identification, and contrast sensitivity.10 These studies shed light on the importance of refractive surgery offered by the DOD.
When analyzing the effect of the COVID-19 pandemic, a decrease in the number of refractive surgery cases performed in the tri-service community was reported. Specifically, the total number of surgeries during fiscal year 2020 was comparable to the number of surgeries in fiscal year 2002, shortly after the procedures were first introduced. The pronounced decrease in the number of surgeries performed was undoubtedly due to factors related to the SARS-CoV-2 pandemic: shutdown of DOD Warfighter Refractive Surgery Centers, unavailability of TDY patients, pre-operative SARS-CoV-2 testing, difficulty with pre-operative virtual briefings, availability of N-95 masks, properly scheduling post-operative follow-up, and limitations on family members helping with patients after surgery. The reduced number of procedures observed in fiscal year 2020 is consistent with many published reports of reduced health care utilization during the COVID-19 pandemic.11 One such report demonstrated initial reduced demand for refractive surgery which subsequently rebounded in 2021.12
In fiscal year 2020, the majority of cases were PRK followed by LASIK/LASEK and SMILE, respectively. A trend toward PRK surgery in the military has been prevalent for years; however, there has been a shift towards LASIK especially among Navy surgery centers.13,14 Various reasons exist for the preference of PRK, which include surgeon's comfort with performing PRK over LASIK, previous military policies that prohibited LASIK for special forces, and the risk of traumatic corneal flap lifting following LASIK that cannot be attended to in an environment that is not readily equipped with an ophthalmologist (e.g., deployment, training, austere environments).15 With the introduction of SMILE in 2016 after the U.S. Food and Drug Administration approval, it has been increasingly implemented in the DOD.16 SMILE has shown promise with comparable, if not better, visual outcomes than PRK and more predictable outcomes and similar corneal biomechanical stability when compared to LASIK.17,18 The emergence of new refractive surgery techniques will continue to provide opportunity for advancement in military refractive surgery.
Limitations of this study include potential bias in data retrieval and documentation. Data were individually reported from each center and were not verified with medical coding. Additionally, refractive surgeries performed outside of Warfighter Refractive Surgery Centers were not captured in this analysis.
In summary, this report demonstrates the trend in refractive surgeries at the DOD Refractive Surgery Centers and reveals the decrease in refractive surgeries during the COVID-19 pandemic. Because of the instrumental role refractive surgery plays in gaining a strategic advantage for the U.S. military warfighter, surgical procedures still continued during this period and will most likely increase to pre-pandemic numbers as the COVID-related restrictions are lifted or conditions to handle COVID-related spread are improved. Future implications from the lessons learned during the COVID-19 pandemic will provide a framework on how to troubleshoot barriers to performing refractive surgery in the future.
Author affiliations: United States Air Force, Medical College of Georgia at Augusta University (2d Lt Brandon Sellers, BS); United States Air Force, Air Force Refractive Surgery Consultant, Joint Base Elmendorf-Richardson, Anchorage, AK (Lt Col J. Richard Townley, MD); United States Navy, Prior Navy Refractive Surgery Program Manager, Camp Lejeune, Jacksonville, NC (CAPT Corby Ropp, DO); United States Army, Army Refractive Surgery Program Manager, Defense Health Agency Refractive Surgery Board Chair, Brooke Army Medical Center, Ft. Sam Houston, TX (LTC Gary Legault, MD). Dr. Corby Ropp died during the creation of this manuscript but was instrumental in compiling the data.
Disclaimer: The contents, views, or opinions expressed in this publication are those of the author(s) and do not necessarily reflect the official policy or position of the Defense Health Agency, Department of Defense, or the U.S. Government.
References
- Lattimore MR, Jr., Schrimsher RH. Refractive error distribution and incidence among U.S. Army aviators. Mil Med. 1993;158(8):553–556.
- Hammond MD, Madigan WP, Jr., Bower KS. Refractive surgery in the United States Army, 2000-2003. Ophthalmology. 2005;112(2):184–190.
- Reynolds ME, Taubman SB, Stahlman S. Incidence and prevalence of selected refractive errors, active component, U.S. Armed Forces, 2001-2018. MSMR. 2019;26(9):26–30.
- Reed DS, Ferris LM, Santamaria J, et al. Prevalence of myopia in newly enlisted airmen at Joint Base San Antonio. Clin Ophthalmol. 2020;14:133–137.
- Sia RK, Ryan DS, Rivers BA, et al. Vision-related quality of life and perception of military readiness and capabilities following refractive surgery among active duty U.S. Military service members. J Refract Surg. 2018;34(9):597–603.
- Legault, GL. Army refractive surgery update. Military Refractive Surgery Safety and Standards Symposium, virtual. 1 January 2021.
- Townley, JR. Air Force refractive surgery update. Military Refractive Surgery Safety and Standards Symposium, virtual. 1 January 2021.
- Ropp, C. Navy refractive surgery update. Military Refractive Surgery Safety and Standards Symposium, virtual. 1 January 2021.
- Reynolds ME, Williams VF, Taubman SB, Stahlman S. Absolute and relative morbidity burdens attributable to ocular and vision-related conditions, active component, U.S. Armed Forces, 2018. MSMR. 2019;26(9):4–11.
- Ryan DS, Sia RK, Stutzman RD, et al. Wavefront-guided versus wavefront-optimized photorefractive keratectomy: Visual and military task performance. Mil Med. 2017;182(1):e1636–e1644.
- Moynihan R, Sanders S, Michaleff ZA, et al. Impact of COVID-19 pandemic on utilisation of health care services: a systematic review. BMJ Open. 2021;11(3):e045343.
- Bickford M, Rocha K. Impact of the COVID-19 pandemic on refractive surgery. Curr Ophthalmol Rep. 2021:1–6.
- Stanley PF, Tanzer DJ, Schallhorn SC. Laser refractive surgery in the United States Navy. Curr Opin Ophthalmol. 2008 Jul;19(4)321–324.
- Gao H, Miles TP, Troche R, et al. Quality of vision following LASIK and PRK-MMC for treatment of myopia. Mil Med. 2021;usab071.
- Shih LY, Peng KL, Chen JL. Traumatic displacement of laser in situ keratomileusis flaps: an integrated clinical case presentation. BMC Ophthalmol. 2021;21(1):177.
- Dishler JG, Slade S, Seifert S, Schallhorn SC. Small-incision lenticule extraction (SMILE) for the correction of myopia with astigmatism: Outcomes of the United States Food and Drug Administration Premarket Approval Clinical Trial. Ophthalmology. 2020;127(8):1020–1034.
- Sia RK, Ryan DS, Beydoun H, et al. Visual outcomes after SMILE from the first-year experience at a U.S. military refractive surgery center and comparison with PRK and LASIK outcomes. J Cataract Refract Surg. 2020;46(7):995–1002.
- Cao K, Liu L, Yu T, Chen F, Bai J, Liu T. Changes in corneal biomechanics during small-incision lenticule extraction (SMILE) and femtosecond-assisted laser in situ keratomileusis (FS-LASIK). Lasers Med Sci. 2020;35(3):599–609.