 A pilot trains in the Research Altitude Chamber 1 at the Air Force Research Laboratory’s 711 Human Performance Wing,Wright-Patterson Air Force Base, Ohio. The RAC can simulate altitudes of up to1,000 feet and is one of four chambers used to study the effects of highaltitudes on humans and equipment. (Photo: Richard Eldridge, U.S. Air Force)
A pilot trains in the Research Altitude Chamber 1 at the Air Force Research Laboratory’s 711 Human Performance Wing,Wright-Patterson Air Force Base, Ohio. The RAC can simulate altitudes of up to1,000 feet and is one of four chambers used to study the effects of highaltitudes on humans and equipment. (Photo: Richard Eldridge, U.S. Air Force)
“We teach both Navy corpsmen and other joint and allied force medics and medical personnel, high-altitude physiology and pathology, or illnesses,” said U.S. Navy Lt. (Dr.) Kevin Lawrence, the officer in charge of the course in mountain medicine.
The three-week-long course is divided into didactic classroom learning, some conditioning, and mobility and technical skills, he said. And since the training center is located on thousands of acres of national forest land with variable elevations, it’s an “ideal” location to train for acclimation, said Lawrence.
“Base camp is at 6,200 feet,” said U.S. Navy Lt. Michael Gumpert, a physician assistant and head of the Branch Health Clinic Bridgeport, Naval Hospital Twentynine Palms. “From there, there are multiple elevations, up to the 10,000-foot level, so there's a lot of variability depending on what the mission set is they're training towards.”
They explained acclimating to high altitude is gradual and passive.
“Between 8,000 feet and 10,000 feet is the first stage for human acclimation at altitude,” said Lawrence. “Visiting units get a couple of days on base to begin their acclimation to altitude so that they can function well as they move into the training area and get to those slightly higher altitudes,” he said.
He added “there's nothing service members can physically do to acclimate faster. People are genetically inclined to either acclimate well or acclimate poorly.”
He also clarified that conditioning is separate from “the actual act of acclimating.”
“Units are expected to be in a high-physical condition, but that doesn't actually allow them to acclimate any faster,” he said.
Medically, Gumpert said lung capacity and being aware of mountain sickness-type symptoms are key factors to pay attention to.
“Besides dealing with higher altitude, it's technically more challenging to accomplish any military mission when you’re also fighting the terrain,” he said.
Acclimating to Altitude
“Anybody can go from sea level to about 8,000 feet in one go with very minimal risk of developing any kind of illness from that 8,000 to 10,000-foot range,” said Lawrence.
To ensure units at MCMWTC don’t develop high-altitude illness, they follow a “step-wide” acclimatization process that includes overnight stays and gradual ascents.
“Studies show that sleeping, the actual overnight sleep portion, is the primary acclimating phase,” he said.
At the MCMWTC, the acclimation process begins on Day 0, where units spend the night at an intermediate altitude, or elevation. On Day 1, units get set up for training and sleep some more.
“Usually, that's sufficient to acclimate most people who are going to be operating up to that 10,000 or 11,000-foot zone,” said Lawrence.
If units need to acclimate farther, “we recommend limited ascents per day, up to about 14,000 feet, and then an additional day to rest,” he explained.
If they need to go above 14,000 feet, they will need to ascend at a slower rate and take more days to rest.
Ranges of Altitude Illness
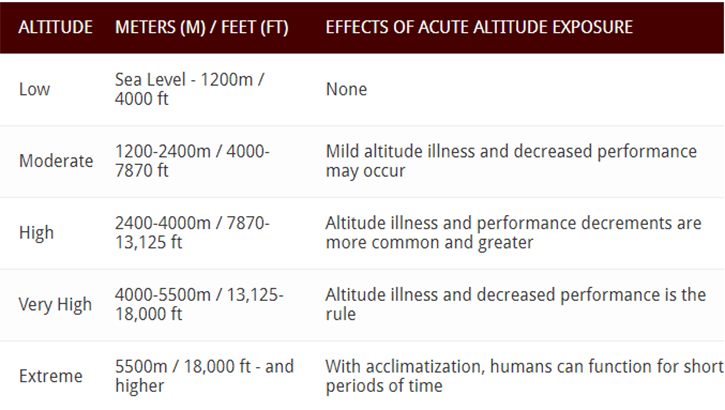
The Army Public Health Center defines the effects of altitude exposure according to different altitude ranges:
Even though units at the MCMWTC usually only experience mild altitude sickness symptoms, there are more severe symptoms that people can develop.
“The more severe end of the spectrum of altitude illness is high-altitude cerebral edema, or brain swelling, and that’s a medical emergency that requires evacuation,” Lawrence said. “But it's rare that it occurs below 11,000 feet.”
He explained this can occur when people ascend too rapidly, not giving their bodies enough time to acclimatize.
“Your body employs a variety of physiologic adaptations to prevent that from happening, but they all take time on the order of a couple of days to really be fully engaged,” he said. “The risk is going from a very low elevation, like that at Twentynine Palms or Camp Pendleton, to suddenly something like 12,000, 14,000, or 16,000 feet in one go.”
In that case, “you haven't given the body time to actually adapt, and you run the risk of more severe altitude illness,” he added.
When that happens, descending to lower altitudes, where there is higher-pressure, is the most effective way to get relief.
At MCMWTC, medical teams use a Gamow Bag, “which is like a mini-deployable pressure chamber where you can increase the air pressure into a moderate degree to try and simulate” an environment with higher pressure, said Lawrence.
Other treatments include supporting patients with a diuretic to help speed the acclimation process, and steroids to help treat the brain swelling and inflammation.
Additional Risks and Symptoms of Altitude Sickness
“The greatest risks associated with high-altitude training and operations are hypoxia, decompression sickness, and barotrauma,” added Reed.
Hypoxia refers to low oxygen levels in your body tissues and occurs when people living at sea level ascend to altitudes above 8,000 feet. Symptoms include confusion, restlessness, difficulty breathing, rapid heart rate, and bluish skin.
Decompression sickness occurs when someone ascends quickly to altitudes above 18,000 feet. The high pressure causes nitrogen to dissolve in the blood and tissues, forming bubbles as pressure decreases. Symptoms can include fatigue and pain in muscles and joints.
Barotrauma refers to injuries, such as of the ear, resulting from steep inclines or descents due to increased air or water pressure during plane flights or scuba diving. With ear barotrauma, the outside pressure is higher than that of the inner ear, causing that stuffy feeling or popping in the ears.
“However, since the factors contributing to these illnesses are well known, a lot of effort is dedicated to mitigation,” said Reed. “Preventive medicine is a major part of treating high-altitude sickness.”
Like Gumpert’s and Lawrence’s teams at MCMWTC, he said that the U.S. Air Force’s flight medicine providers and technicians “routinely screen and assess aircrew for any predisposing conditions,” highlighting that those medics are “specifically trained” to diagnose and provide specialty care for such instances.
For more information on the effects of high-altitude, check out how the Army developed a tool to save lives at high altitude. To learn more about acclimating to high altitudes, talk to your health care provider.