Abstract
Central serous chorioretinopathy (CSCR) is a condition that affects central visual function. It can produce blurred and/or distorted vision that can impact the performance of military duties. CSCR can recur in susceptible individuals. Incident cases of CSCR among active component service members were found to average 18.3 per 100,000 person-years (p-yrs) during 2001–2018. Incidence rates increased during the surveillance period by 60.7% and were more common with increasing age. Overall rates of incident CSCR diagnoses were highest among Air Force (20.7 per 100,000 p-yrs) and Navy members (19.9 per 100,000 p-yrs) and lowest among Marine Corps members (12.5 per 100,000 p-yrs). Pilot/air crew occupational groups had rates almost twice that of other groups. Annual recurrence rates increased 71.4% over the course of the 18-year period.
What Are the Findings?
This is the first MSMR report of the incidence of CSCR among members of the U.S. Armed Forces. More than 4,400 individuals received incident diagnoses of CSCR during the 18-year surveillance period. Rates of incident CSCR diagnoses and rates of recurrent diagnoses increased from 2001 through 2018. Across the services, overall rates of CSCR were highest among those in pilot/air crew occupations, with comparable rates observed among Navy members in combat related occupations.
What Is the Impact on Readiness and Force Health Protection?
CSCR can affect critical visual performance by degrading central visual acuity. The acute disease typically lasts about 3 months, leading to operational limitations. Even after the resolution of acute symptoms, residual effects on vision may remain. Recurrences are commonly reported and may result in prolonged periods of non-deployability or non-retainability of service members.
Background
Central serous chorioretinopathy (CSCR) is caused by fluid under the retina in the subretinal space. Fluid accumulation causes anatomic and functional changes affecting visual function. Typical symptoms include objects appearing smaller than normal (micropsia), straight lines appearing wavy (metamorphopsia), or partial loss or distortion of a portion of the central visual field. Symptoms may be more subtle as well and can include loss of contrast sensitivity (the ability to distinguish between bright and dim parts of an image) and color saturation.1 CSCR is the fourth most common cause of retinopathy after age-related macular degeneration, diabetic retinopathy, and branch retinal vein occlusion. CSCR is a significant cause of both temporary and permanent loss of visual function among individuals aged 30–50 years.1,2
Although the etiology of CSCR remains poorly understood, a number of risk factors for the condition have been identified. Increased cortisol from either exogenous or endogenous sources has been associated with increased risk of developing CSCR.3,4 Development of CSCR has often been associated with a "Type A" behavior pattern.5 CSCR most commonly is a self-limiting condition, with resolution of retinal changes and return to baseline visual acuity within 3 months.1 The condition can recur, and recurrences of CSCR have been reported in up to one-half of patients within 1 year.6 Some patients may have a more prolonged course of the disease, with 15% of patients having signs and symptoms lasting longer than 6 months (chronic CSCR).7
The best available estimate of the incidence rates of CSCR in the U.S. comes from a population-based retrospective study in Olmstead County, MN, during 1980–2002.8 This study reported an overall incidence rate of 5.8 per 10,000 persons. Age-adjusted incidence was 9.9 per 100,000 persons among men and 1.7 per 100,000 persons for women.8 The reported male-to-female ratio ranged from 2.2:1 to 5.7:1.8 These numbers are reported in both population-based retrospective cohort studies and case-control studies.8 The current report summarizes the frequencies, rates, and temporal trends of CSCR among active component service members during 2001–2018.
Methods
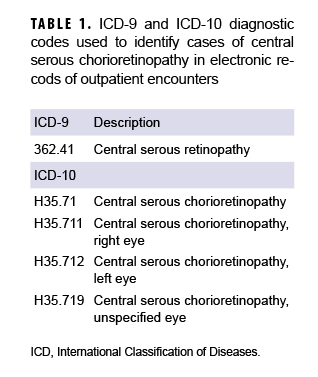
The surveillance period was 1 Jan. 2001 to 31 Dec. 2018. The surveillance population included all individuals who served in the active component of the U.S. Army, Navy, Air Force, or Marine Corps at any time during the surveillance period. Diagnoses of CSCR were ascertained from records maintained in the Defense Medical Surveillance System (DMSS) that document outpatient encounters of active component service members. Such records reflect care in fixed military treatment facilities of the Military Health System (MHS) and in civilian sources of health care underwritten by the Department of Defense.
International Classification of Diseases (ICD) codes for the case-defining diagnoses of CSCR are shown in Table 1. For surveillance purposes, an incident case was defined by at least 1 outpatient medical encounter with a qualifying diagnosis in any diagnostic position. The incidence date was the date of the first qualifying outpatient encounter and an individual was counted as an incident case only once per lifetime. Person-time at risk included all active component military service time before the date of incident diagnosis, termination of military service, or the end of the surveillance period, whichever came first. Incidence rates were calculated as incident CSCR diagnoses per 100,000 person-years (p-yrs). Prevalent cases (i.e., service members with case-defining diagnoses occurring before the start of the surveillance period) were excluded from the analysis.
Recurrent cases of CSCR were identified using a 120-day gap rule in that there had to be at least 120 days of no outpatient diagnoses for CSCR before the next case could be counted. Incident cases were not included in the analysis of recurrent cases. The person-time at risk for the analysis of recurrent cases included active component military service time from the incident case diagnosis to termination of military service or the end of the surveillance period, whichever came first.
Results
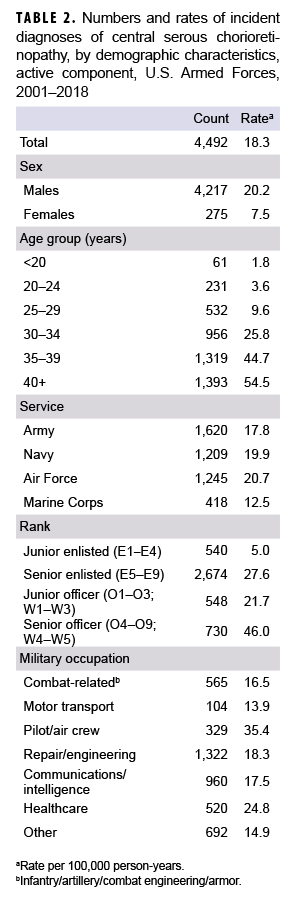
During 2001–2018, incident diagnoses of CSCR averaged 18.3 per 100,000 p-yrs (Table 2). The crude overall incidence rate of CSCR diagnoses among males was more than 2.5 times that among females (20.2 per 100,000 p-yrs and 7.5 per 100,000 p-yrs, respectively). Overall rates increased markedly with increasing age, with the rates among service members 40 years or older almost 30 times the rate among those less than 20 years old. This age distribution is consistent with the finding of the highest rates among the most senior rank group (O4–O9 and W4–W5).
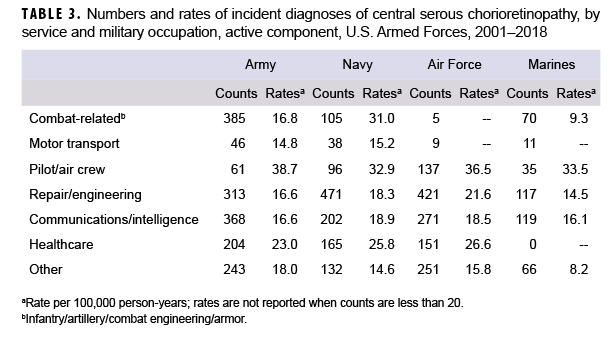
Across the services, overall rates of incident CSCR diagnoses were highest among Air Force (20.7 per 100,000 p-yrs) and Navy members (19.9 per 100,000 p-yrs) and lowest among Marine Corps members (12.5 per 100,000 p-yrs). Overall rates among military occupational groups showed considerable variation, with service members in the pilot/air crew occupations having a rate almost 2 times the rates of those in other occupational groups (with the exception of health care). Service members working as pilots/air crew had the highest overall incidence rates of CSCR diagnoses in all 4 of the services (Table 3). Of note, within the combat-related occupations, Navy members had an overall incidence rate 1.8 and 3.3 times that of Army and Marine Corps members, respectively. Service members in health care occupations had the second highest overall rate of incident CSCR diagnoses during the surveillance period.
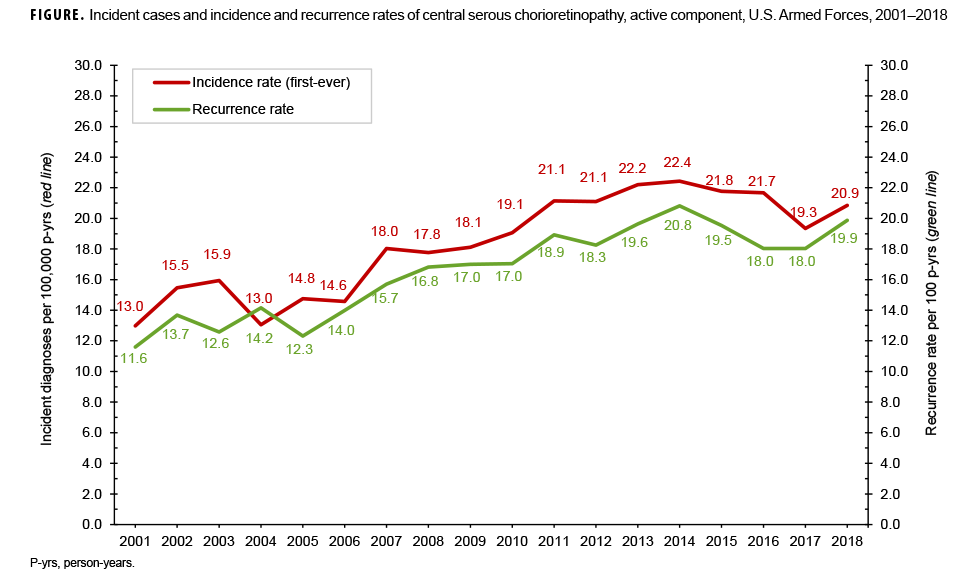
Crude annual rates of incident CSCR diagnoses increased during the surveillance period by 60.7% and fluctuated between a low of 13.0 per 100,000 p-yrs in 2001 and a high of 22.4 per 100,000 p-yrs in 2014 (Figure). Annual recurrence rates increased 71.4% over the course of the 18-year period. The largest increase in recurrence rates over time was seen among members of the Marine Corps, and the smallest increase was observed among Navy members (data not shown).
Editorial Comment
This is the first MSMR report focused on the incidence and distribution of CSCR among active component service members. Compared to previously reported rates of CSCR in U.S. civilian populations,8 rates among the active component were higher for both men and women, with male-to-female ratios within the previously reported ranges (male rate 2.7 times that of female). These elevated incidence rates are not directly comparable because of differences in methodology (e.g., the rates in this report are described in p-yrs, while the rates in other reports are per 100,000 people). Despite this comparability issue, the elevated rates may represent a unique risk factor profile for active component service members or increased recognition and diagnosis in the population.
The higher rates of incident CSCR diagnoses seen among service members working in pilot/air crew occupations are notable. These occupations have strictly defined visual function requirements across all services. In previous reports of CSCR among military aviators, service members with single episodes of CSCR usually recovered vision within aviation standards, but recurrences were more likely to result in permanent visual changes.9 The increased rates found among Navy combat-related occupational groups warrants further investigation.
An important consideration when interpreting increasing incidence rates of CSCR diagnoses is the advance in diagnostic capabilities. Optical coherence tomography (OCT), a diagnostic modality that provides a cross-sectional view of the retina, was developed in 1991.10 OCT is frequently used to diagnosis and monitor CSCR and has increased in fidelity since it was first introduced.11 The increased availability and utilization of OCT over the course of the surveillance period should be taken into account when interpreting the reported increased rates.
An additional limitation of the current analysis is related to the implementation of MHS GENESIS, the new electronic health record for the MHS. Medical data from sites that were using MHS GENESIS were not available in the DMSS. These sites include Naval Hospital Oak Harbor, Naval Hospital Bremerton, Air Force Medical Services Fairchild, and Madigan Army Medical Center. Therefore, medical encounters and person-time data for individuals seeking care at any of these facilities during 2017 and 2018 were excluded from the analysis. This is notable since Madigan Army Medical Center has a retina service that would be expected to be a referral center for patients with CSCR. Despite a possible attenuation of counts and rates, this report provides critical epidemiological information concerning this important ocular condition.
Acknowledgments: The authors would like to acknowledge the vitreoretinal specialist review by LTC Marissa L Wedel, MC, USA.
Author affiliations: Department of Defense/Veterans Affairs Vision Center of Excellence, Defense Health Agency Research and Development Directorate (COL Reynolds); contract personnel in support of the Department of Defense/Veterans Affairs Vision Center of Excellence (Dr. Karesh); Armed Forces Health Surveillance Branch, Defense Health Agency (Mr. Oh, Dr. Stahlman)
Disclaimer: The contents, views, or opinions expressed in this publication are those of the author(s) and do not necessarily reflect the official policy or position of the Defense Health Agency, Department of Defense, or the U.S. Government.
References
- Liew G, Quin G, Gillies M, Fraser-Bell S. Central serous chorioretinopathy: a review of epidemiology and pathophysiology. Clin Exp Ophthalmol. 2013;41(2):201–214.
- Wang M, Munch IC, Hasler PW, Prunte C, Larsen M. Central serous chorioretinopathy. Acta Ophthalmol. 2008;86(2):126–145.
- Garg SP, Dada T, Talwar D, Biswas NR. Endogenous cortisol profile in patients with central serous chorioretinopathy. Br J Ophthalmol. 1997;81(11):962–964.
- Haimovici R, Koh S, Gagnon DR, Lehrfeld T, Wellik S. Risk factors for central serous chorioretinopathy: a case–control study. Ophthalmology. 2004;111(2):244–249.
- Liu B, Deng T, Zhang J. Risk factors for central serous chorioretinopathy: a systematic review and meta-analysis. Retina. 2016;36(1):9–19.
- Aggio FB, Roisman L, Melo GB, Lavinsky D, Cardillo JA, Farah ME. Clinical factors related to visual outcome in central serous chorioretinopathy. Retina. 2010;30(7):1128–1134.
- Gilbert CM, Owens SL, Smith PD, Fine SL. Long-term follow-up of central serous chorioretinopathy. Br J Ophthalmol. 1984;68(11):815–820.
- Kitzmann AS, Pulido JS, Diehl NN, Hodge DO, Burke JP. The incidence of central serous chorioretinopathy in Olmsted County, Minnesota, 1980–2002. Ophthalmology. 2008;115(1):169–173.
- Green RP Jr, Carlson DW, Dieckert JP, Tredici TJ. Central serous chorioretinopathy in U.S. Air Force aviators: a review. Aviat Space Environ Med. 1988;59(12):1170–1175.
- Huang D, Swanson EA, Lin CP, et al. Optical coherence tomography. Science. 1991;254(5035):1178–1181.
- Staurenghi G, Sadda S, Chakravarthy U, Spaide RF. Proposed lexicon for anatomic landmarks in normal posterior segment spectral-domain optical coherence tomography: the IN•OCT consensus. Ophthalmology. 2014;121(8):1572–1578.