What Are the New Findings?
The yearly incidence of animal-related injuries to U.S. Army VS personnel did not change significantly from 2001–2018. Dog bites were the most common type of animal-related injury. Being female, younger, and a veterinary technician were all associated with an increased risk for animal-related injury.
What Is the Impact on Readiness and Force Health Protection?
Risk of injury among VS personnel varied by sex, age, and occupation. Leaders within the VS must ensure that there are no disparities in training or equipping the veterinary force to handle animals properly and that animal-related injury prevention measures are in place and prioritized.
Abstract
Limited data exist on animal-related injuries in the U.S. Army veterinary service (VS). The purpose of this study was to determine the incidence of animal-related injuries and the associated risk factors in VS personnel. A retrospective cohort study was conducted using military health care surveillance data on animal-related injuries in VS personnel from 2001–2018. Yearly incidence of medically diagnosed animal-related injuries ranged from 25–50 injuries per 1,000 person-years from 2001–2018. Linear regression showed no significant trend in the incidence rate per year over the study period (R²=0.005). Bites were the most common injury (86.5%), with dog bites (44.3%) being the most common injury type and dogs the most common species implicated. After controlling for sex, age group, race/ethnicity group, and occupation, adjusted incidence rate ratios (AIRRs) showed significantly elevated risk for animal-related injuries among females compared to males (AIRR=1.69; 95% confidence interval [CI]: 1.45–1.99), soldiers aged 17–29 compared to those aged 30 years or older (AIRR=2.55; 95% CI: 2.12–3.08), and technicians compared to veterinarians (AIRR=1.57; 95% CI: 1.30–1.89). Unlike the majority of published literature on veterinary occupational health and safety, this study showed a clear increased risk of diagnoses of injury among females compared to males.
Background
The U.S. Army veterinary service (VS) comprises enlisted soldiers serving as animal care specialists and veterinary food inspection specialists, veterinary corps officers (VCOs: veterinarians and food safety officers), and Department of the Army civilians. The VS serves as the lead organization for the animal health mission within the Department of Defense (DOD). This mission includes, but is not limited to, the clinical and surgical care of military working dogs (MWDs), DOD-owned animals used in research, and the privately owned pets of DOD service members and their beneficiaries.
Because of the broad responsibilities and specialized skill sets of veterinarians and veterinary technicians, there are unique occupational risks related to animal exposure. Physical injuries from an animal by a bite, scratch, or other physical strike during restraint, treatment, or handling are the most common circumstances for veterinary occupational injuries. In the civilian community, animal-related injuries to veterinarians and technicians have been well documented.1–7 Data on the prevalence or incidence and associated risk of animal-related injuries to U.S. Army VS personnel are limited, however. Between 2001 and 2010, 433 (2.1%) of the approximately 20,000 animal bites to service members were to VS personnel.8 In a more recent publication, of the approximately 22,000 animal bite cases among reserve and active component service members during 2011–2018, 537 (2.4%) were among VS personnel. The crude incidence rate of animal bites in VS personnel was 438 per 100,000 person-years (p-yrs) from 2011 through 2018. This incidence rate was second only to the rate of animal bites among service members working in military law enforcement.9 These data on U.S. Armed Forces pertained to animal bites only and did not show specific incidence rates for demographic, occupational, or military subgroups of service members within the VS (i.e., age groups, sex, veterinarians vs. technicians, junior enlisted vs. senior enlisted).
In the veterinary profession, animal bites and scratches can be frequent and their severity can range from requiring only basic first aid to necessitating hospitalization. Furthermore, these injuries have a high probability of causing secondary wound infections and/or long-term disabilities.1,2,4 It has been estimated that between 50%–67% of veterinarians and up to 98% of veterinary technicians have had an animal-related injury during their careers.4 Musculoskeletal diseases and other conditions secondary to or indirectly related to animal exposure and work are also common within the veterinary community. These exposures may include heavy lifting, repetitive motions, anesthetic gases, x-rays, needle stick injuries, and a variety of toxic pesticides and therapeutic agents.10–12
For the purposes of this study, animal-related injuries were limited to those caused by mammalian species and do not include injuries from venomous reptiles or arthropods. The specific type of animal-related injury varies by frequency and risk, depending upon the predominant mammalian species with which a veterinary professional is working. Overall, the most dangerous animals to work around are cattle and horses. Injuries caused by these large mammalian species account for the most human fatalities and are responsible for many serious crush and kick injuries.2,5 One survey-based study of members of the American Association of Swine Practitioners reported that needle stick injuries were the most common type of animal-related injury and that 22% of swine practitioners reported having a diagnosis of hearing impairment.13 Small animal practitioners' animal-related injuries are mostly confined to dog and cat bites and/or scratches. However, there is variability between studies on the prevalence and severity of dog vs. cat bites and/or scratches.1–7
VS personnel have the most experience and are the subject matter experts in animal handling and animal-related safety for the DOD. To maintain their expertise in this field, and in order to train others on safe animal handling practices, the VS needs to ensure that their methods are as safe and effective as possible. Increasing the overall readiness of VS soldiers requires a targeted training approach for risk mitigation of animal-related injuries. Determining the most at-risk members of the VS population could inform the development, refinement, and targeted implementation of prevention strategies to further reduce animal-related injuries within the VS.
The purpose of this study was to determine the incidence of medically documented animal-related injuries among active component VS personnel from 2001 through 2018 and the associated risk factors. Based on a review of the published literature and experience in the VS, it was hypothesized that young age, male sex, and occupation as a technician would be associated with an increased risk for animal-related injuries within this population.
Methods
This report describes a retrospective cohort study of active component VS soldiers and VCOs from 1 Jan. 2001 through 31 Dec. 2018. Deidentified demographic and medical encounter data were provided by the Armed Forces Health Surveillance Branch of the Defense Health Agency. Institutional Review Board (IRB) approval was obtained from the Uniformed Services University IRB. Service members with U.S. Army military occupational specialty (MOS) codes 91T and 68T (animal care specialists, hereafter referred to as technicians) and all 64 series (64A, 64B, 64C, 64D, 64E, 64F, 64Z, hereafter referred to a veterinarians) constituted the population of interest.
Animal-related injury events (cases) were identified from inpatient and outpatient encounter data among garrison-stationed VS personnel and did not include deployed or in-theater cases. Each active component VS member with a medical encounter that included a diagnostic code indicative of an animal-related injury (i.e., nonvenomous mammal bite, scratch, or other nonvenomous mammalian-related injury type) in any diagnostic position within the described surveillance period was defined as a case. Case-defining codes included International Classification of Diseases, 9th Revision (ICD-9) codes E906.0, E906.1, E906.3, E906.5, E906.8, and E906.9 and International Classification of Diseases, 10th Revision (ICD-10) codes W53.*, W54.*, and W55.*.
After a diagnosis met the definition of a case, any subsequent diagnosis of an animal-related injury was not counted as an incident case unless at least 90 days had passed since the prior diagnosis with the same animal-related injury–defined ICD code or the subsequent ICD code was different from the prior animal-related injury ICD code. This criterion reduced the likelihood of double counting cases who were receiving follow-up care for the original injury. Person-time sums for the populations of technicians and veterinarians during the study period were calculated overall, by year, and by demographic variables. The demographic variables describing each member of the cohort were the following: MOS (91T/68T or 64 series), age group (17–19, 20–29, 30–39, and 40+ years), sex (male or female), and race/ethnicity group (non-Hispanic white, non-Hispanic black, Hispanic, Asian/Pacific Islander, American Indian/Alaska Native, and other/unknown), and rank/grade (junior enlisted [E1–E4], senior enlisted [E5–E9], junior officer [O3–O4], and senior officer [O5–O10]).
Grade/rank was not included as a variable for calculating risk because the definitions of the rank categories are not appropriate to the ranks of VCOs. Because of relatively small cell sizes in the youngest and the oldest age groups, combined age groups of 17–29 years and 30 years or older were created. Similarly, the "non-Hispanic black" and "other/unknown" race/ethnicity groups were combined to allow for comparison to the non-Hispanic white group. This simplification allowed for a binomial assessment of all demographic parameters (i.e., male vs. female, veterinarian vs. technician, old vs. young, and white vs. non-white).
Descriptive statistics were used to analyze the incidence rates of animal-related injuries according to the demographic variables within the populations of technicians and veterinarians. Animal bites with ICD-9 codes that were not indicative of a dog or rat (ICD-9: E906.3 and E906.5) or with ICD-10 codes that were not indicative of a dog, rat, cat, horse, cow, hoof stock, pig, or raccoon (ICD-10: 55.81*) were classified as "other". Each type of animal-related injury was totaled by species and injury type to the highest specificity allowed by ICD coding. Injury counts by type and species were presented as totals and percentages of all injuries in the cohort during 2001–2018. Yearly incidence rates for the study period were calculated by dividing the total number of incident cases for each year by the sum of p-yrs for that year. Incidence rates were calculated as incident animal-related injury diagnoses per 1,000 p-yrs. The linear trendline function in Microsoft Excel for Office 365 was used to assess the fit (R2) of a regression line to the annual incidence rates over time (2018, Microsoft Corporation, Redmond, WA).
Multivariable Poisson regression models were used to calculate adjusted incidence rate ratios (AIRRs) and 95% confidence intervals (CIs) controlling for sex, combined age group, combined race/ethnicity group, and occupation. Statistical significance was defined as p < .05. With the exception of the simple trendline assessment, statistical analyses were carried out using Stata/IC, version 15 (2015, StataCorp LLC, College Station, TX).
Results
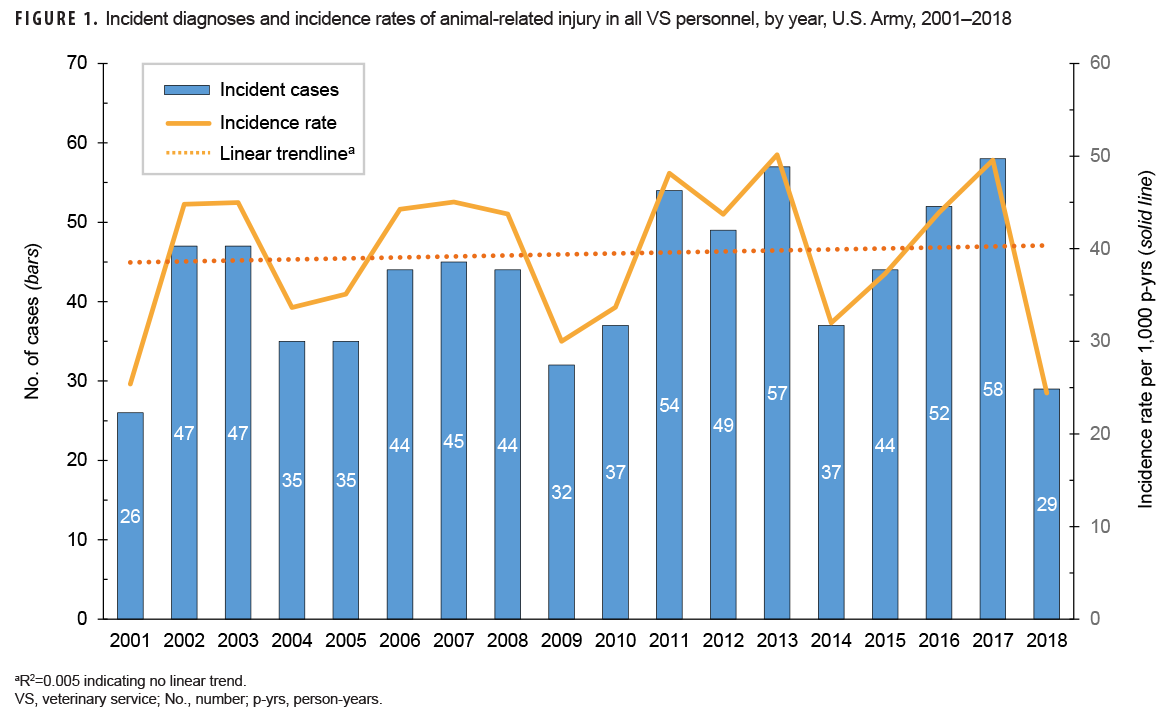
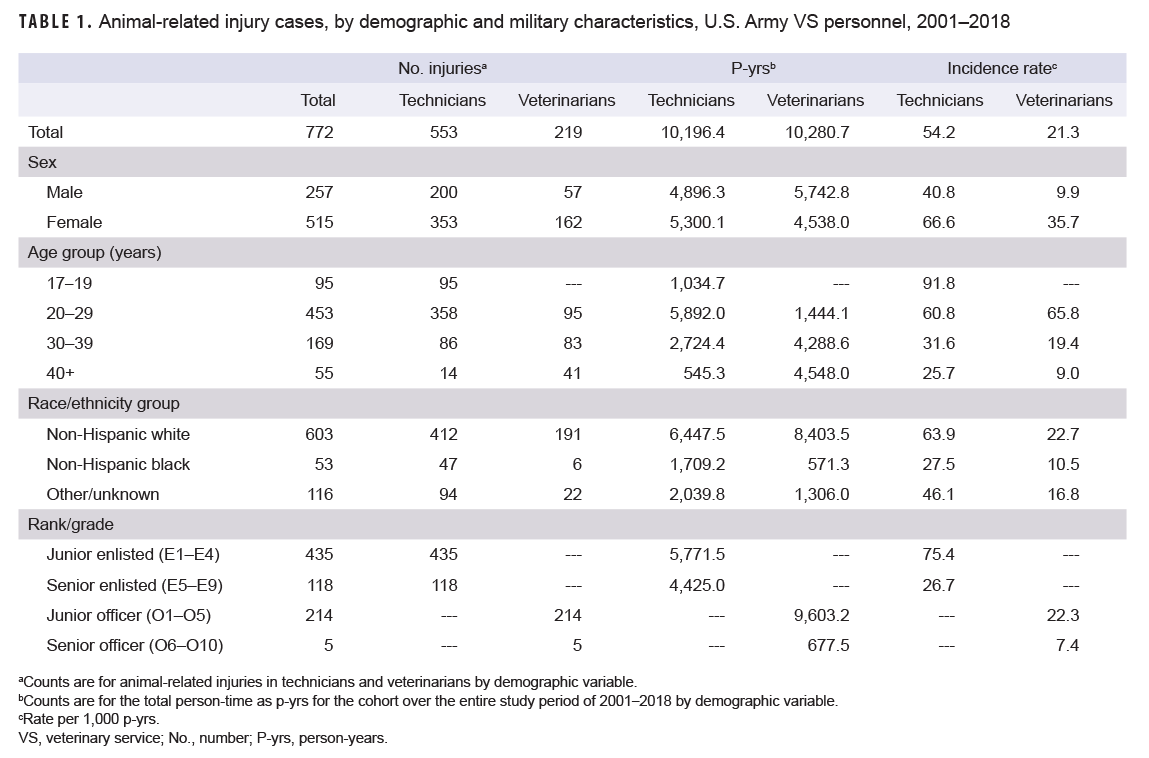
A total of 772 incident animal-related injury diagnoses were ascertained among VS personnel from 2001 through 2018, resulting in an overall incidence rate of 37.7 per 1,000 p-yrs (Table 1). The subgroup with the highest crude incidence rate was technicians aged 17–19 years, at 91.8 injuries per 1,000 p-yrs. During the surveillance period, approximately 43 incident animal-related injuries were diagnosed per year among VS personnel, with the lowest counts of injuries in 2001 (n=26) and the highest in 2017 (n=58) (Figure 1). Examination of crude incidence rates of animal-related injury diagnoses over time showed no linear trend (R2=0.005); annual rates fluctuated between 50.1 per 1,000 p-yrs in 2013 and 24.4 per 1,000 p-yrs in 2018 (data not shown). Compared to their respective counterparts, technicians, females, those in younger age groups, non-Hispanic white VS personnel, and junior enlisted soldiers had the highest crude rates for animal-related injuries (Table 1).
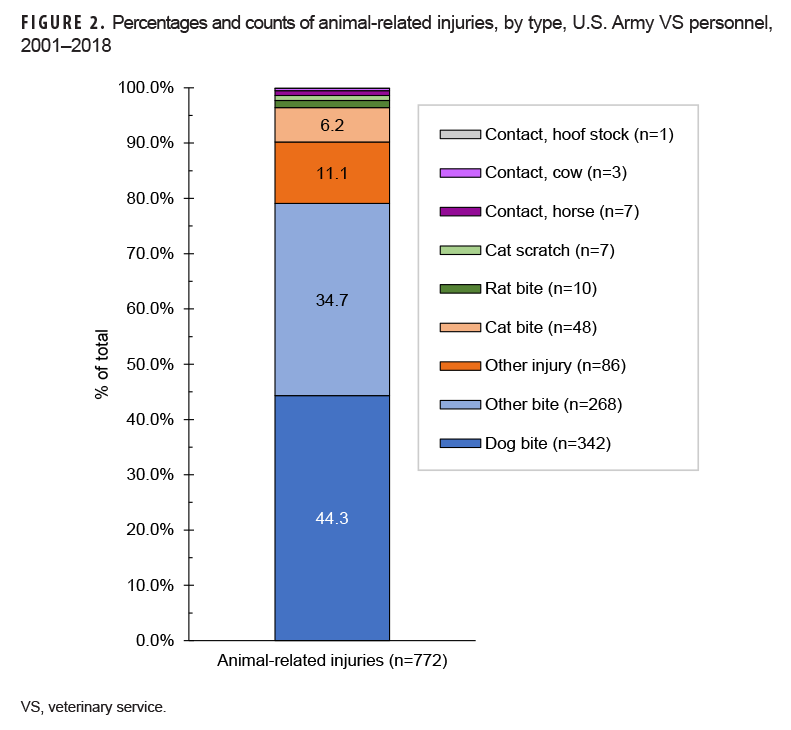
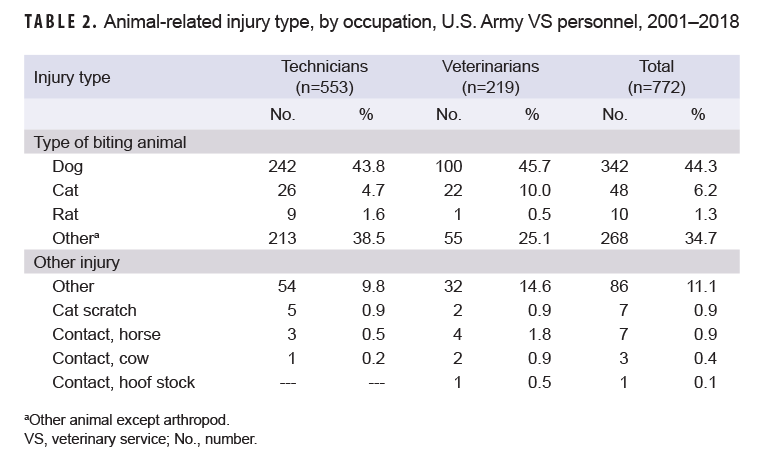
Of all injuries counted, 668 (86.5%) were bites from a variety of species (Table 2, Figure 2). Of all the animal-related injuries, dog bites were the single most common type, with a total of 342 (44.3%). "Other" bites accounted for 34.7% (n=268) of the total. Only 11 recorded injuries were caused by large-bodied mammal species. Of the 772 total injuries, 553 (71.6%) were sustained by veterinary technicians, while only 219 (28.4%) were sustained by veterinarians. The majority of animal-related injuries were among females (n=515; 66.7%) (Table 1). Of the technicians' injuries, 435 (78.7%) were in junior enlisted soldiers, and of the veterinarians' injuries, 214 (97.7%) were in junior officers. More than three-quarters (78.1%) of the animal-related injuries were among non-Hispanic white soldiers.
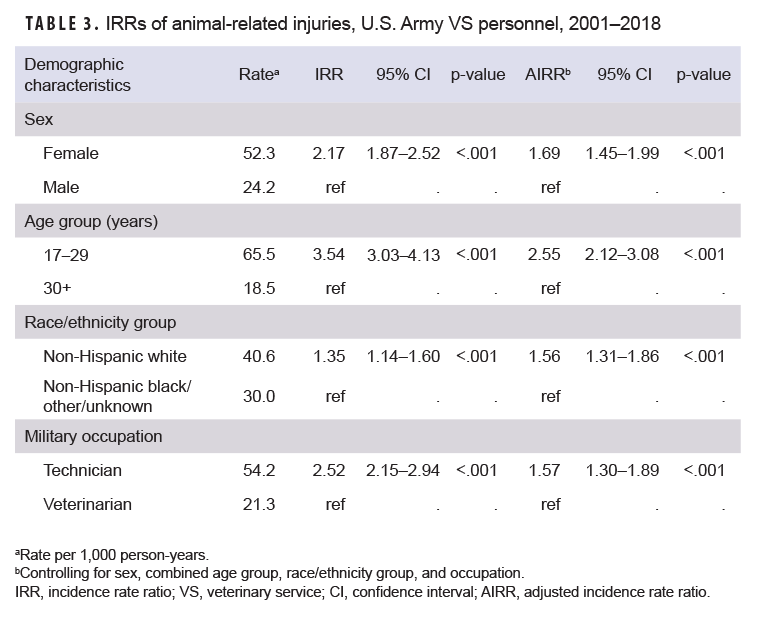
Unadjusted IRRs revealed a more than 2-fold increased risk in sustaining a diagnosis of an animal-related injury for females vs. males (IRR=2.17; 95% CI: 1.87–2.52), technicians vs. veterinarians (IRR=2.52; 95% CI: 2.15–2.94), and those 17–29 years old vs. those 30+ years old (IRR=3.54; 95% CI: 3.03–4.13) (Table 3). After adjustment for sex, age, race/ethnicity, and occupation, these differences in rates remained statistically significant. Even after combining minority race/ethnicity categories, non-Hispanic white soldiers showed a 56% increased incidence of animal-related injury compared with the combined non-Hispanic black/other/unknown group in the adjusted model (AIRR=1.56; 95% CI: 1.31–1.86) (Table 3).
Editorial Comment
The results of this study indicate that technicians, females, and younger soldiers were at a higher risk of sustaining an animal-related injury when compared to veterinarians, males, and older soldiers, respectively. Even in the adjusted analysis, there was at least a 50% increase in risk for younger individuals, technicians, and females when compared to older individuals, veterinarians, and males, respectively (Table 3). The explanation for the increased risk observed in females compared to males is not immediately apparent. In VS clinical operations, males are frequently selected for riskier tasks involving the handling of aggressive animals because of physical stature or strength. Furthermore, the "white male effect" has been previously described in risk perception literature, showing that white males tend to perceive less risk than women and minorities.14 If the perception of risk is higher in females than in males in the VS cohort described here, it was not reflected in a decreased rate of animal-related injuries for females. An additional potential explanation for the increased risk of injury to female compared to male VS personnel may be related to differences in their health care-seeking behavior. Health behavior literature cites that females are more likely to utilize health care services than males, and it is possible that the increased incidence of injuries in females is a reporting bias due to their increase in health care seeking behavior.15
One survey of Canadian veterinarians showed an increase in the odds of injury for females compared to males.10 However, in an Australian veterinary injury study, Lucas and colleagues found that even with the increase in female veterinarians in the profession, a larger percentage of animal-related injuries was found in males.2 To date, a literature search has not found a study describing the relationship of sex with animal-related injuries among veterinary technicians. Nordgren and colleagues6 discussed work-related risk factors for animal-related injuries in certified veterinary technicians. However, they were unable to include sex in their statistical models because 97% of the study participants were female.
An increased risk for technicians to sustain an injury in the VS is conceivable, as technicians work with many more animals and would have more animal contact than a veterinarian. An increased risk of an animal-related injury for technicians when compared to veterinarians is well documented in the published literature.1,3,4
Several previous studies have shown that younger age increases the risk of sustaining an animal-related injury.6,8,9,12 Regarding the increased rate of animal-related injuries in younger service members, this finding could be related to experience and work type. Junior enlisted soldiers and junior officers generally have more direct animal contact than their superiors. The frequency of animal contacts decreases dramatically as a VS soldier increases in rank (and consequently age), and the chance of injury is simply decreased as a result. Furthermore, those who have served in their career field longer may be less likely to suffer injuries or to seek medical care for injuries because they perceive them as minor. Moreover, junior soldiers might be directed or required to seek care for an injury by their superiors, whereas a more senior soldier may be able to more readily decline medical attention.
Previous research has described the type of animal-related injury by species and veterinary practice type.4,5,7,10,13 VS clinical operations can be described as a mostly "small animal practice" for civilian veterinary clinic comparisons. In the civilian population, Fowler and colleagues4 found that cats were the most likely species to cause an injury in small animal practice.4,6 However, other studies have found that the highest incidence of animal-related injuries in small animal clinics is attributable to dogs.2,16 The number of cat-related injuries in the VS cohort during 2001–2018 was 55 (48 bites and 7 scratches). Unfortunately, the granularity of ICD-9 codes were unable to indicate cats as a species type. The incident cases of cat-related injuries counted in this study were counted from 2015–2018, following the introduction of ICD-10 coding into the Military Health System. As a result, many "other" bites from before 2015 may have been cat bites that were not identifiable as such.
The present study had a very specific population definition that is demographically unique compared to civilian small animal veterinary clinics. The uniqueness of this population makes it difficult to generalize the results and make statistical comparisons to other cohort, case control, or cross-sectional studies regarding animal-related injuries in veterinary professionals. The most significant differences between this study and published literature on the topic are the roughly equal numbers of females and males within the population studied and the identification of female gender as a risk factor. Therefore, the analysis discussed here is unique in that gender was able to be evaluated as a risk factor in animal-related injuries within the veterinary profession.
Unfortunately, there is no way to know the number of animal-related injuries for which the VS personnel did not seek health care. Presumably, most animal-related injuries in VS service members are very minor, and the medically diagnosed incidence rates calculated here are very likely to be an underestimation of the true injury burden.9 Self-treatment and lack of injury reporting in veterinary professionals have been previously described.1,4,13,17,18 The change in ICD coding from ICD-9 to ICD-10 in 2015 altered the categorical or species type of some injuries and made it difficult to determine total and accurate risk by animal species for the entire surveillance period. Another limitation regarding animal information would be the &"type"of species with respect to VS-specific mission sets. For example, of the 342 dog bites found in this study, it is unknown how many of those bites were from MWDs or other government-owned animals compared to privately owned animals. The type of species causing most animal-related injuries in VS personnel is a key piece of information that needs to be studied in order to effectively focus training on mitigation strategies and policies for improved workplace safety.
No inferences can be made about specific VS billets and their risk (i.e., garrison VS duties vs. lab animal research vs. a field unit). ICD-10 coding contains occupational injury codes that could have been utilized in the inclusion criteria. However, this could have possibly excluded many cases, and that designation did not exist for all ICD-9 codes. Therefore, occupational codes were not used in this analysis and there was no definitive way to determine if the injury was truly occupational in nature. In addition, there may be a significant differential misclassification bias if many more females than males reported animal-related injuries. This bias could result in falsely increasing the strength of association found.
The present study showed that there is an increased risk for diagnosed animal-related injury in females compared to males, young soldiers compared to older, and technicians compared to veterinarians in the VS population. VS leadership should utilize these data to ensure that there are no gender disparities in the training programs for animal care specialists (MOS 68T). Furthermore, leadership should ensure that there are no disparities in the duty assignments of female VS personnel or in the onsite training and task management of new female technicians. Additional research needs to be completed, along with task-specific and MOS-specific military injury data, in order to determine if changes need to be made for the entry requirements of the 68T MOS. Commanders and VCOs should utilize this information to ensure that their technicians, especially young female service members, utilize the appropriate personal protective measures and follow all safety protocols and standard operating procedures in order to mitigate animal-related injury risk.
Acknowledgments: The authors would like to thank Ms. Sorana Raiciulescu and MAJ Craig Calkins for their masterful spreadsheet and statistical support, without which this project would certainly not have been possible.
Author affiliations: U.S. Army Medical Research Institute of Chemical Defense, Veterinary Medicine and Surgery Department (MAJ Messenger); Armed Forces Health Surveillance Branch (Dr. Stahlman); Fort Drum Army Medical Department Activity Chief of Preventive Medicine, Uniformed Services University of the Health Sciences, Department of Preventive Medicine and Biostatistics, Assistant Professor (MAJ Chern).
Disclaimer: The contents of this publication are the sole responsibility of the authors and do not necessarily reflect the views, opinions, or policies of Uniformed Services University of the Health Sciences, the Department of Defense, or the Departments of the Army, Navy, or Air Force. Mention of trade names, commercial products, or organizations does not imply endorsement by the U.S. Government.
References
- Nienhaus A, Skudlik C, Seidler A. Work-related accidents and occupational diseases in veterinarians and their staff. Int Arch Occup Environ Health. 2005;78(3):230–238.
- Lucas M, Day L, Shirangi A, Fritschi L. Significant injuries in Australian veterinarians and use of safety precautions. Occup Med (Lond). 2009;59(5):327–333.
- Fowler HN, Holzbauer SM, Smith KE, Scheftel JM. Survey of occupational hazards in Minnesota veterinary practices in 2012. J Am Vet Med Assoc. 2016;248(2):207–218.
- Fowler H, Adams D, Bonauto D, Rabinowitz P. Work-related injuries to animal care workers, Washington 2007–2011. Am J Ind Med. 2016;59(3):236–244.
- Barros N, Langley R. Fatal and non-fatal animal-related injuries and illnesses to workers, United States, 2011–2014. Am J Ind Med. 2017;60(9):776–788.
- Nordgren LD, Gerberich SG, Alexander BH, Church TR, Bender JB, Ryan AD. Evaluation of factors associated with work-related injuries to veterinary technicians certified in Minnesota. J Am Vet Med Assoc. 2014;245(4):425–433.
- Poole AG, Shane SM, Kearney MT, Rehn W. Survey of occupational hazards in companion animal practices J Am Vet Med Assoc. 1998;212(9):1386–1387.
- Armed Forces Health Surveillance Center. Animal bites, active and reserve components, U.S. Armed Forces, 2001–2010. MSMR. 2011;18(9):12–15.
- Williams VF, Taubman SB, Stahlman S. Animal bites and rabies post-exposure prophylaxis, active and reserve components, U.S. Armed Forces, 2011–2018. MSMR. 2019;26(10):13–20.
- Epp T, Waldner C. Occupational health hazards in veterinary medicine: physical psychological, and chemical hazards. Can Vet J. 2012;53:151–157.
- Elbers ARW, Blaauw PJ, de Vries M, et al. Veterinary practice and occupational health: an epidemiological study of several professional groups of Dutch veterinarians. Vet Q. 1996;18(4):127–131.
- Gabel CL, Gerberich SG. Risk factors for injury among veterinarians. Epidemiology. 2002;13(1):80–86.
- Hafer A, Langley RL, Morrow MWE, Tulis JJ. Occupational hazards reported by swine veterinarians in the United States. Swine Health and Production. 1996;4(3):128–141.
- Kahan DM, Braman D, Gastil J, Slovic P, Mertz CK. Culture and identity-protective cognition: explaining the white male effect in risk perception. J Empir Leg Stud. 2007;4(3):465–505.
- Bertakis KD, Azari R, Helms LJ, Callahan EJ, Robbins JA. Gender differences in the utilization of health care services. J Fam Pract. 49(2):147–152.
- Langley R. Animal bites and stings reported by United States Poison Control Centers 2001–2005. Wilderness Environ Med. 2008;19(1):7–14.
- Parkin TDH, Brown J, Macdonald EB. Occupational risks of working with horses: a questionnaire aurvey of equine veterinary surgeons. Equine Vet Educ. 2018;30(4):200–205.
- Reijula K, Rasanen K, Hamalainen M, et al. Work environment and occupational health of Finnish veterinarians. Am J Ind Med. 2003;44(1):46–57.