What Are the New Findings?
LARC use continued to increase among service women through 2019. Use decreased in 2020 possibly due to the COVID-19 pandemic. Differences in prevalence and continuation by demographics highlight important areas for further research and provider awareness.
What Is the Impact on Readiness and Force Health Protection?
LARCs are highly effective and long-acting birth control that can improve service women's overall health and readiness. LARCs are available in a variety of clinics both on and off base.
Abstract
Long-acting reversible contraceptives (LARCs) are highly effective means of birth control that can improve service women's overall health and readiness. This report expands upon prior data and summarizes the annual prevalence (overall and by demographics) of LARC use from 2016 through 2020 among active component U.S. service women, compares LARC prevalence to the prevalence of short-acting reversible contraceptives (SARCs), and evaluates the probability of continued use of LARCs by type. LARC use increased from 21.9% to 23.9% from 2016 through 2019 while SARC use decreased from 28.3% to 24.9%. Both SARC and LARC use decreased in 2020 which may have been related to the coronavirus disease 2019 (COVID-19) pandemic. The prevalence of intrauterine devices (IUDs) was greater than implants, and IUDs also had a higher probability of continuation than implants. At 12 months, the continuation for IUDs was 81% compared to 73% for implants. At 24 months, the probabilities of continuation were 70% for IUDs and 54% for implants. Probabilities of continuation were similar across outsourced care and Click to closeDirect CareDirect care refers to military hospitals and clinics, also known as “military treatment facilities” and “MTFs.”direct care settings. The increased use of LARCs along with their high frequency of continuation in U.S. service women may have a positive impact on overall health and readiness.
Background
Women need access to safe and effective forms of contraception for family planning, treatment of menstrual disorders, and if desired, for menstrual suppression. These needs hold true for women in the military as well, whether it be for career planning, deployments, or due to unique job demands. A recent study found that female officers reported the desire for menstrual suppression during training.1 In response to concerns from the Assistant Secretary of Defense for Health Affairs regarding the health care and readiness of female service members, the Defense Health Board (DHB) released a report in November 2020 recommending improved contraceptive education and services, particularly access to long-acting reversible contraceptives (LARCs).2 This recommendation stemmed from studies reporting that service women have an unintended pregnancy rate 50% higher than civilians and studies demonstrating lower unintended pregnancy rates among women with access to LARCs.2
LARCs are well established as the most effective form of reversible contraception with a typical use failure rate of <1% compared to 4–7% for short-acting reversible contraceptives (SARCs).3 The rate of unintended pregnancies in the U.S. has decreased by 18% since LARC use became more common in the early 2000s.4 LARCs have become more commonly used largely because no ongoing effort is required of the patient, and once the device is removed, fertility rapidly returns. LARCs are considered safe and have few contraindications. Aside from providing effective contraception, some LARCs effectively manage menstrual irregularities and can be used for menstrual suppression. The 2 types of LARCs available in the U.S. are the intrauterine device (IUD) and the implant. These devices can stay in place for 3–10 years depending on the product. However, some women experience side effects such as irregular bleeding that lead them to have the devices removed.
U.S. service women have universal access to health care, including contraceptive counseling and services, at no personal cost. In 2017, Stahlman et al. evaluated the use of contraceptives in service women from 2012 through 2016.5 This study found that more than three-quarters (76.2%) of active component U.S. service women of childbearing potential used either a LARC or SARC.5 During the study period, LARC use increased from 17.2% to 21.7% while SARC and sterilization use decreased.5 LARC use was most common among service women 25–29 years old, American Indian/Alaska Native women, Hispanic women, senior enlisted personnel, those in health care occupations, and those with "other/unknown" marital status.5 A study on LARC use in all military beneficiaries found that 74.6% of women who initiated LARCs selected IUDs.6 Women were more likely to continue IUDs than implants, although overall continuation of LARCs was high. LARC discontinuation was more common in women aged 20–24, those using an implant, and those initiating LARCs in military clinics (versus outsourced care).6
Despite the advantages of LARCs, their use remains relatively low. The goal of this study was to assess the current status of LARC use in U.S. service women and expand upon the findings of previous studies of this population. The first objective was to determine the annual prevalence of LARC compared to SARC use in active component women from 2016–2020 and evaluate differences in LARC use by demographic groups. The second objective was to evaluate whether discontinuation of LARCs inserted from 2016 through 2019 differed by LARC type and other covariates present at the time of insertion.
Methods
This study used a retrospective cohort design. The surveillance period was 1 Jan. 2016 through 31 Dec. 2020. The study population consisted of all active component service women aged 17 or older who served in the Army, Navy, Air Force, or Marine Corps at least 1 day during the surveillance period.
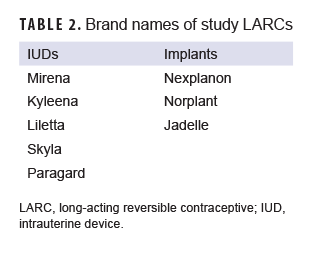
All data used for analyses were derived from the Defense Medical Surveillance System (DMSS) which includes data for all active duty service members.7 The prevalence of LARC and SARC coverage by calendar year was estimated using methods similar to those of a prior MSMR report.5 Service members were identified as using LARCs or SARCs using the following criteria: 1) receipt of a prescription for contraception (per American Hospital Formulary Service Pharmacologic-Therapeutic Class: 681200 or 683200); 2) or International Classification of Diseases, 9th and 10th Revision, Clinical Modification (ICD-9/10-CM) procedure (Table 1), diagnosis, or Current Procedural Terminology (CPT) code for insertion documented in a record of an inpatient or outpatient medical encounter. LARCs included IUDs and implants, whereas SARCs included oral contraceptives, patches, vaginal rings, and injectables.
Women were considered to be covered by a LARC in a given calendar year if they had a filled prescription for 1 of the contraceptives listed in Table 2 and/or an ICD code for insertion without removal code for a LARC. A removal with reinsertion code or a same day removal and insertion was considered to be the insertion of a new LARC. Periods of contraceptive coverage were created based on the FDA-approved coverage period for a given contraceptive type during the surveillance period. IUDs were assigned a default 5-year coverage period; however, Skyla IUDs were assigned a 3-year coverage period and ParaGard IUDs were assigned a 10-year coverage period. Implants were assigned a default 3-year coverage period except for both Norplant® and Jadelle implants, which were assigned a 5-year coverage period. Coverage ended on the date that the implant or IUD was removed, based on documentation of a removal in ICD diagnostic, procedural, or CPT codes, or at the end of the coverage period. For SARCs, service members who had a filled prescription at any point during the calendar year were considered covered for that year.
Women were counted in the denominator as long as they were in the active component at least 1 day during the calendar year. Women were only counted as being covered by a LARC or SARC during a calendar year if they were also in the denominator for that calendar year. If a woman had both IUD and implant coverage for a given year, the IUD was prioritized over the implant. In addition, if they had both a LARC and a SARC, the LARC was prioritized.5 Time-dependent variables, such as age and military rank, were determined at the end of each calendar year. A service member was considered deployed if she had at least 1 deployment of 30 days or greater length during that calendar year.
Descriptive statistics were used to characterize the overall proportion of women utilizing LARCs and SARCs, and the proportion by age group, race/ethnicity group, military rank, service branch, military occupation, educational level, and whether or not they had a deployment during the surveillance period. Data were stratified by calendar year. Poisson regression with robust error variance was used to calculate adjusted prevalence ratios for LARC use compared to no LARC use for calendar year 2020. The model included age group, race/ethnicity group, military rank, service branch, marital status, education level, military occupation, and whether or not women were deployed in 2020. The reference groups were those aged 17–19, non-Hispanic White women, single women, those with a high school education or less, Army members, junior enlisted women, those in communications career fields, and those with no deployment.
For the second objective, a time-to-event analysis was performed to assess probability of continuation for LARCs among women who had a LARC inserted between 2016 and 2019. Women who had a LARC inserted in 2020 were excluded to ensure that all women in the analysis had at least 1 year of follow-up time. This analysis only included women with a first-ever insertion encounter during that time period. Service women were followed for up to 3 years after LARC insertion until either removal of the LARC or loss to follow-up. Loss to follow-up was defined as leaving military service or the end of the surveillance period, 31 December 2020, whichever came first. Time to event analyses were stratified by age group, race/ethnicity group, rank, service, military occupation, marital status, education level, and insertion site.
Results
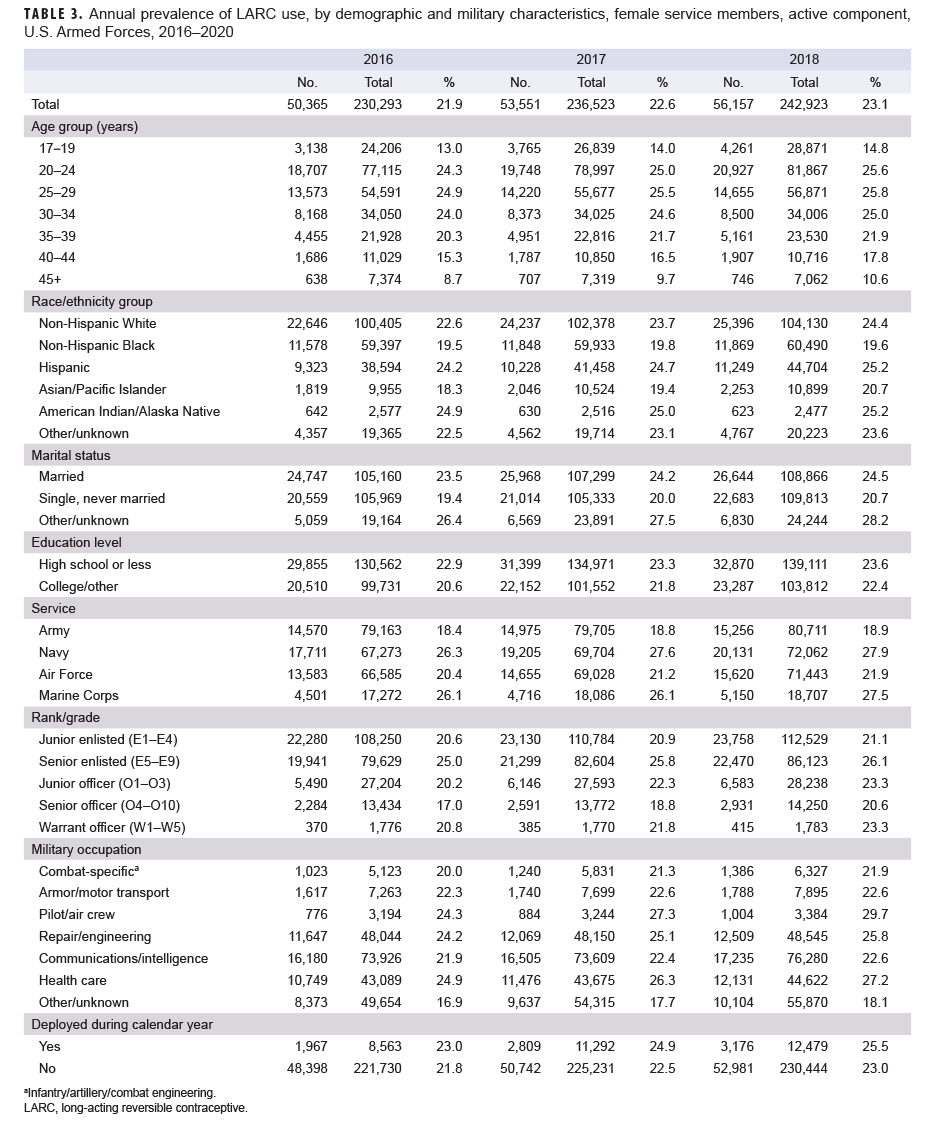
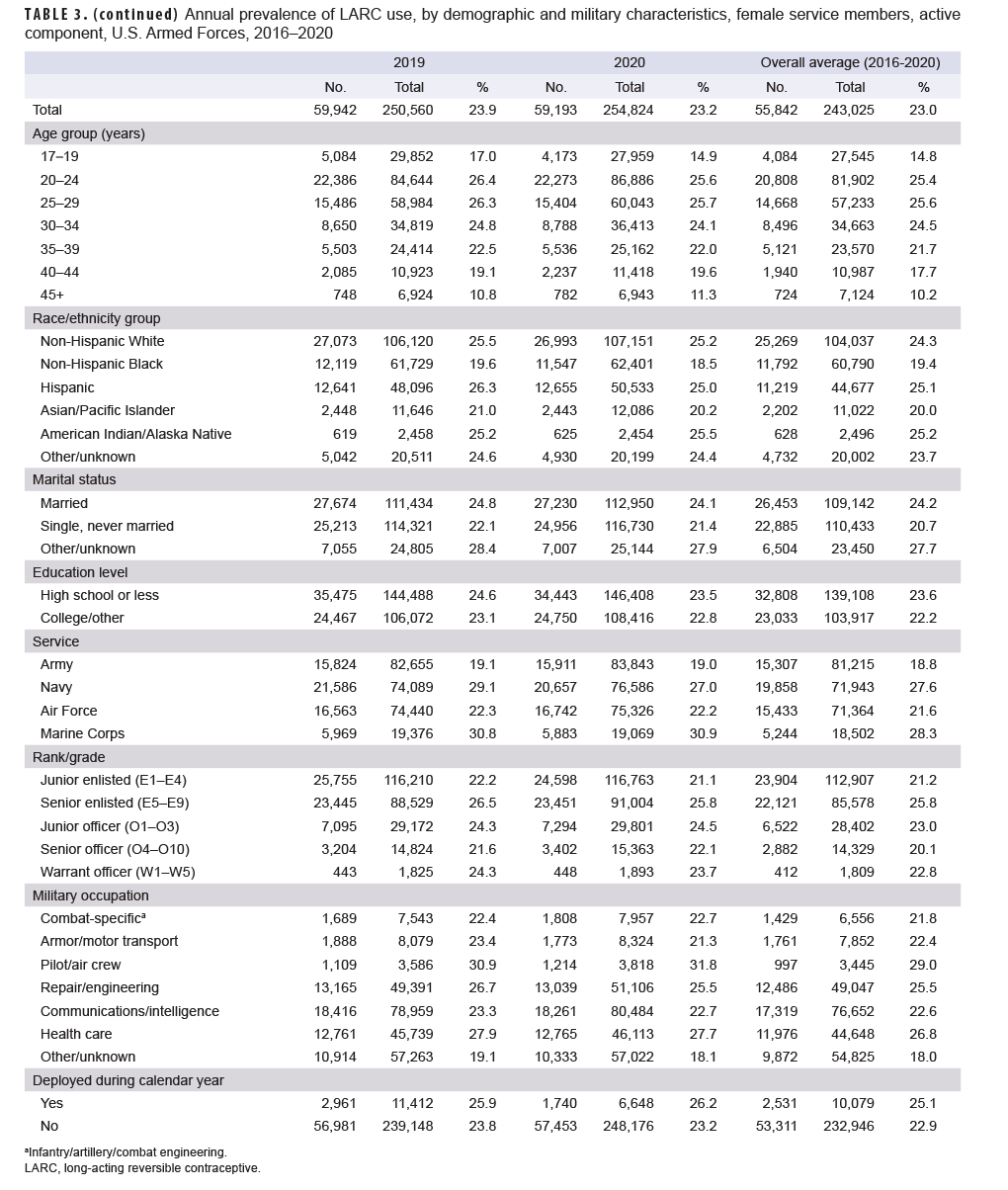
There were on average 243,025 women who served in the active component of either the Army, Navy, Air Force, or Marine Corps in a given calendar year between 2016 and 2020 (Table 3). In 2016, 50,365 (21.9%) of these women used LARCs with use increasing to 59,942 (23.9%) in 2019 before dropping to 59,193 (23.2%) in 2020 with an average annual prevalence of 23.0%. LARC use trended up through 2019 in almost all demographic categories. During this same time period, SARC use trended down from 65,121 (28.3%) in 2016 to 58,379 (22.9%) in 2020 (Figure 1). Overall combined LARC or SARC use trended down from 50.2% in 2016 to 46.1% in 2020.
Overall, LARC users were most likely to be aged 20–34, senior enlisted, and "other" marital status (Table 3). There was a notable increase (4.3%) in LARC use over time by women 40 years or older. Prevalence was highest among non-Hispanic White, Hispanic, and American Indian/Alaska Native service women. Use increased in Asian/Pacific Islander service women over the course of the study period, but remained relatively constant in non-Hispanic Black service women. Unlike other race/ethnicity groups, and all other demographic groups, non-Hispanic Black service women's LARC use was relatively stable over the surveillance period (Figure 2). Use of LARCs was more prevalent among members of the Navy and Marine Corps followed by the Air Force and Army. By 2020, LARC use was most prevalent among service women in pilot/air crew occupations followed by those in repair/engineering occupations. Women with a high school education had slightly higher prevalence of LARC use compared to women with a college education. In addition, women with a deployment during the calendar year had a slightly higher prevalence of LARC use.
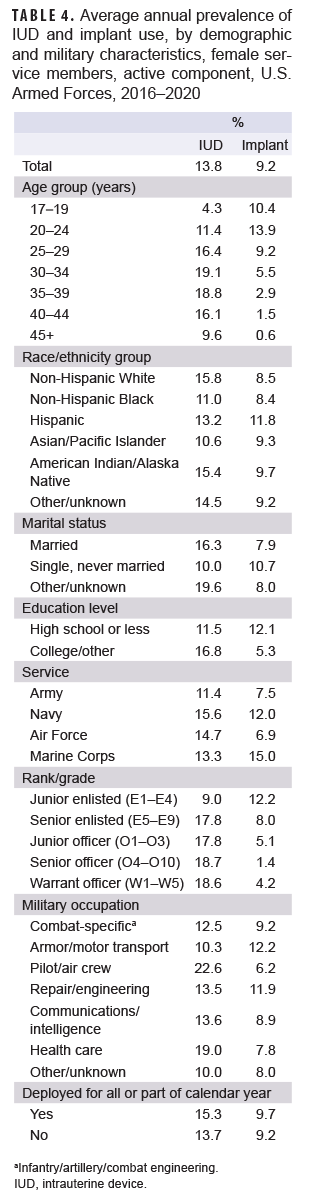
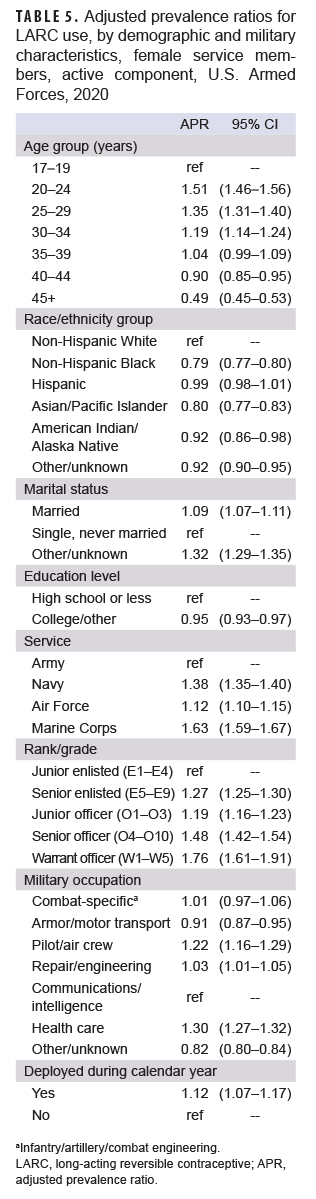
Use of IUDs was more prevalent than implants with an average overall prevalence of 13.8% for IUDs compared to 9.2% for implants (Table 4). Both IUD and implant use increased slightly until 2019 before dropping in 2020 (Figure 1). IUD use was more prevalent in women in their 30s, officers, those with a college education, and women in the Air Force and Navy (Table 4). Implant use was more prevalent in younger, single marital status, junior enlisted, and Hispanic service women. Implants were also most prevalent in the Marine Corps followed by the Navy as well as the armor/motor transport and repair/engineering career fields. The adjusted findings from the multivariable model demonstrated similar patterns as the unadjusted prevalence analysis with some findings reaching statistical significance (Table 5).
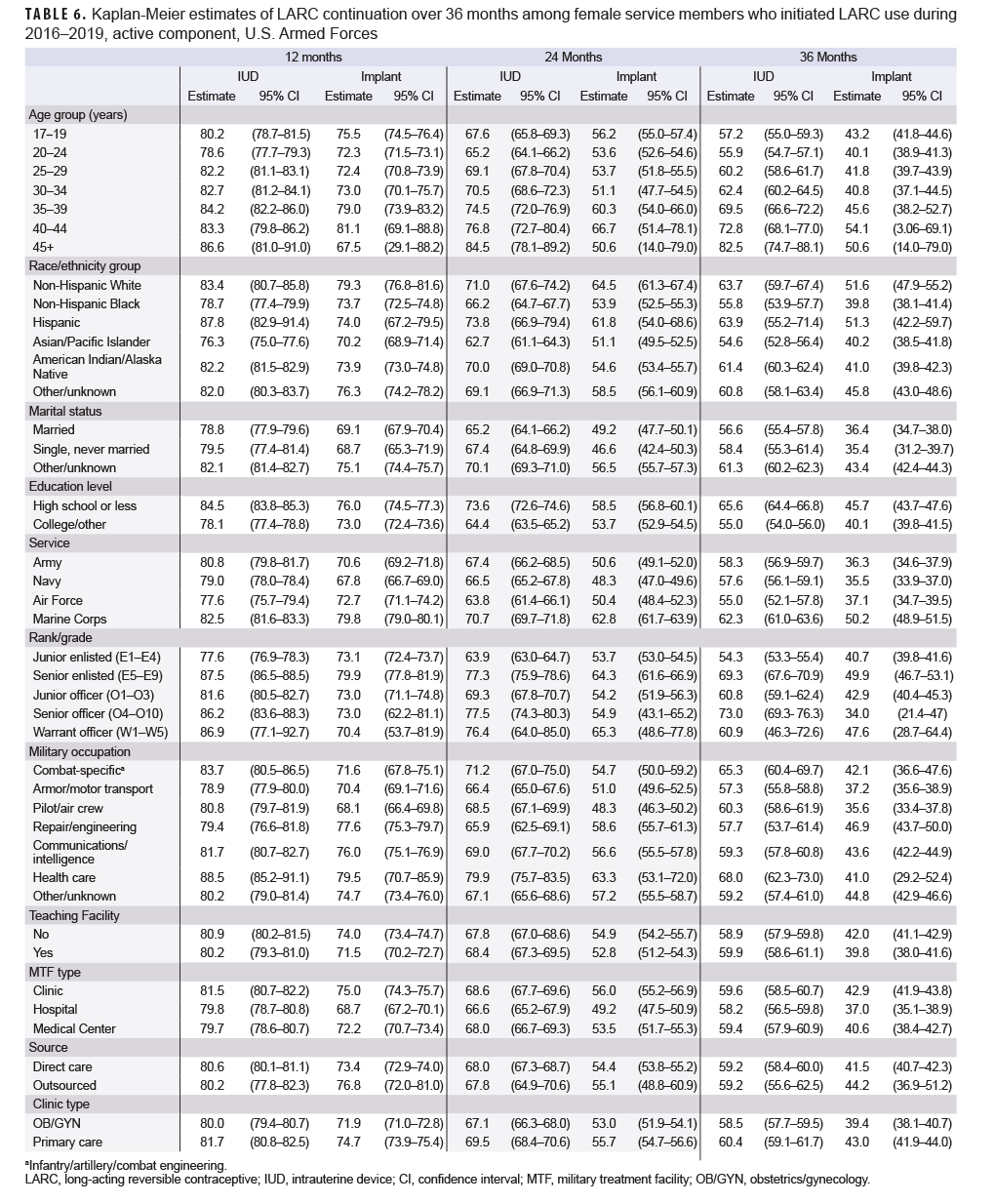
Survival analyses showed that service women had a higher probability of continuing IUD use compared to implants (Figure 3). At 12 months, the continuation for IUDs was 81% compared to 73% for implants. At 24 months, the probability of continuation was 68% for IUDs and 54% for implants. Continuation dropped to 59% for IUDs and 42% for implants at 36 months, at which point most implants need to be removed or replaced. Women over 35 and women who were single had the highest continuation for both types of LARCs, compared to their respective counterparts at the 36-month point (Table 6). Asian/ Pacific Islander, Native American/Alaska Native women, and other women had higher implant continuation while Native American/Alaska Native, Asian/Pacific Islander, non-Hispanic White, and other women had higher IUD continuation. Notably, non-Hispanic Black women had the lowest LARC prevalence as well as the lowest continuation rates. In contrast, Hispanic women had high LARC utilization but low continuation compared to other race/ethnicity groups. Service women in the Navy had much higher continuation of implants and IUDs compared to those in the other services. Pilot/air crew had the highest continuation of both IUDs and implants, compared to those in other occupations. Combat-specific occupations also had high rates of continuation for IUDs. For implants, women working in health care and communications/intelligence had the lowest continuation. Finally, LARC continuation was higher in those with a college education and also for officers and warrant officers versus enlisted members.
Similar probabilities of continuation were observed for LARCs inserted in outsourced care and direct care settings (Table 6). For both IUDs and implants inserted in a military treatment facility (MTF) (direct care), continuation was longer for LARCs inserted in primary care clinics versus obstetrics/gynecology (OB/GYN) clinics. For IUDs, continuation was similar among MTF type; however, implant continuation was longer if inserted at a clinic or medical center compared to a hospital. Continuation was similar for both types of LARCs whether or not they were inserted at teaching facilities.
Editorial Comment
This report summarizes the prevalence of LARC use and continuation for active component service women between 2016 and 2020 and expands upon the findings of previous studies. LARC use overall and among almost all demographic groups increased through 2019 but decreased in 2020. This decline may have been due to the coronavirus disease 2019 (COVID-19) pandemic, as women may have avoided coming in for appointments during this time. Additionally, there were limitations on appointments and types of procedures being performed during the pandemic. SARC use decreased as LARC use increased during the study period; however, it is unclear whether the increase in LARC use fully accounted for the decrease in SARC use as combined contraceptive use declined over this time period.
This study also found that LARC use during the surveillance period was more prevalent in service women than U.S. civilian women, with an average annual prevalence of 23.0% compared to 10.4%, respectively.8 One explanation for this difference could be the universal and free access to health care in the military, which could make service women more likely to take advantage of these services. Age patterns of women using LARCs were similar for service women and civilian women, although use differed by education level, with LARC use being more prevalent among civilian women with a higher education level compared to those with a high school education.8 However, service women with higher education levels did have a higher prevalence of LARC use compared to civilian women of a similar education level. This difference could be because the majority of service women are enlisted which does not require a college degree. Civilian studies showed no difference by race/ethnicity group in LARC use; however, both this study and a similar study in military populations did show differences.5,8,9 The cause for this divergence is unclear. Institutional or personal biases could limit the contraceptive options offered to these women.10,11 These patient populations may also not be choosing LARCs for some reason, such as distrust of the health care system.10,11
Among active component service women, LARC use was more prevalent in the Navy and Marine Corps with those in the Navy also having high continuation. This finding may be a result of the Navy actively working to increase awareness and access to contraception.12 Certain career fields seem to prefer the use of LARCs, and in particular, LARC use was high in pilots and air crew, as well as in health care personnel. Pilot/air crews deploy frequently and spend long hours in aircraft that may not afford them access to convenient restrooms. Additionally, women in these fields may be grounded for part or all of their pregnancies. Therefore, they have an incentive to use highly effective contraception and for menstrual suppression. Health care workers may be more knowledgeable regarding their options for medical care because of the nature of their jobs.
Continuation among active component service women in this study was overall lower than what has been seen in the U.S. population,13 and slightly lower than that seen in prior studies of military health system (MHS) populations.5,6 However, it should be noted that all of these studies were conducted differently so direct comparisons are challenging. This study did not exclude women who removed their LARC due to desire for pregnancy. This study also included only active component service members and not all MHS beneficiaries. Continuation was higher for IUDs versus implants and this may be due to the side effect profiles, although this study did not assess reason for discontinuation. Other studies also showed higher continuation for IUDs compared to implants.5,6,13 Continuation was lower in younger women and those with lower education level, which has also been noted in other studies in both the U.S. and the MHS.6,13 Lower continuation could be due to providers not explaining efficacy and side effects at a level appropriate to the patient's health literacy.
Both the current study and a U.S. study showed racial differences in continuation.13 A prior study of all female MHS beneficiaries showed higher continuation in outsourced care, but that was not the case for this study.6 This study also found minimal differences in continuation among LARCs inserted at military treatment facilities (MTF) of different sizes, teaching facilities, and clinics. These findings suggest that women have access to LARCs at facilities of all sizes with both primary care and OB/ GYN providers, and in both outsourced and direct care.
This study had several limitations. Retrospective data were used to estimate coverage periods and assumptions about how long a LARC remained inserted could have resulted in incorrect coverage periods. Because this study utilized administrative health care data, there was the potential for misclassification of LARC coverage or discontinuation due to inaccurate coding. The type of IUD or implant (e.g., Paragard, Nexplanon) could only be distinguished using pharmacy records, which were sometimes missing. In addition, the reason for LARC removal could not be determined (e.g., desiring pregnancy compared to discomfort or dissatisfaction with the LARC).
Overall, this study found that LARC use in active component U.S. service women is increasing with relatively high continuation especially for IUDs. U.S. service women have higher utilization of LARCs than their civilian counterparts. However, this study highlights the need to continue to promote LARC use in U.S. service women which includes ensuring proper education on efficacy and side effects as well as increased awareness about where LARCs can be obtained. The Air Force Medical Service (AFMS) needs to ensure there are adequate numbers of providers at all facilities to counsel patients about contraception and place LARCs. Future studies could evaluate patient comfort with male providers as well as LARC use and prevalence stratified by gender of provider as well as clinic model (e.g., a traditional clinic versus a walk-in model).
Further evaluation should be undertaken to investigate trends such as the high prevalence of use in the Navy, racial/ethnic differences seen in the military but not the U.S. population, reasons as to why certain career fields favor LARCs, and reasons for discontinuation. The findings of this study can be utilized to individualize care for certain patient populations such as by age or occupation. Minimal difference in continuation was noted by insertion site which means that women have access to LARCs in a variety of medical facilities and in both primary care and OB/GYN clinics. These findings highlight the role of primary care clinics in providing LARC services. Ensuring such clinics are fully staffed is vital for women's health care. Finally, even in a global pandemic, access to effective birth control remains important and should be considered when determining essential medical services.
Author Affiliations: Department of Preventive Medicine and Biostatistics, Uniformed Services University, Bethesda, MD (Lt Col Lotridge); Epidemiology and Analysis, Armed Forces Health Surveillance Division, Silver Spring, MD (Drs. Chauhan, Patel, and Stahlman, Ms. Mcquistan, CAPT Wells).
Disclaimer: The opinions and assertions expressed herein are those of the author(s) and do not necessarily reflect the official policy or position of the Uniformed Services University or the Department of Defense.
References
- Ricker EA, Goforth CW, Barrett AS, Deuster PA, de la Motte SJ. Female Military Officers Report a Desire for Menstrual Suppression During Military Training. Mil Med. 2021;186(Suppl 1):775–783.
- Defense Health Board. Active Duty Women's Health Care Services. https://health.mil/About-MHS/OASDHA/Defense-Health-Agency/Defense-Health-Board/Reports. Published 5 November 2020. Accessed 16 March 2021.
- Centers for Disease Control and Prevention. Contraception. https://www.cdc.gov/reproductivehealth/contraception/index.htm. Updated 13 August 2020. Accessed 24 March 2021.
- Practice Bulletin No. 186: Long-Acting Reversible Contraception: Implants and Intrauterine Devices. Obstet Gynecol. 2017;130(5):e251–e269.
- Stahlman S, Witkop CT, Clark LL, Taubman SB. Contraception among active component service women, U.S. Armed Forces, 2012–2016. MSMR. 2017;24(11):10–21.
- Chiles DP, Roberts TA, Klein DA. Initiation and continuation of long-acting reversible contraception in the United States military health care system. Am J Obstet Gynecol. 2016;215(3):328.e321–329.
- Defense Medical Surveillance System. https://www.health.mil/Military-Health-Topics/Combat-Support/Armed-Forces-Health-Surveillance-Branch/Data-Management-and-Technical-Support/Defense-Medical-Surveillance-System. Updated February 2017. Accessed 24 March 2021.
- Daniels K, Abma JC. Current Contraceptive Status Among Women Aged 15–49: United States, 2017– 2019. NCHS Data Brief. 2020(388):1–8.
- Kramer RD, Higgins JA, Godecker AL, Ehrenthal DB. Racial and ethnic differences in patterns of long-acting reversible contraceptive use in the United States, 2011–2015. Contraception. 2018;97(5):399–404.
- Thorburn S, Bogart LM. Conspiracy Beliefs About Birth Control: Barriers to Pregnancy Prevention Among African Americans of Reproductive Age. Health Educ Behav. 2005;32(4):474–487.
- Thorburn S, Bogart LM. African American Women and Family Planning Services: Perceptions of Discrimination. Women health. 2005;42(1):23–39.
- Navy and Marine Corps Public Health Center. Women's Health and Readiness. https://www.med.navy.mil/sites/nmcphc/health-promotion/womens-health/Pages/default.aspx. Accessed 6 April 2021.
- Diedrich JTMDM, Zhao QMS, Madden TMDMPH, Secura GMP, Peipert JFMDP. Three-year continuation of reversible contraception. Am J Obstet Gynecol. 2015;213(5):662.e661–662.e668.