Abstract
This report provides an update through June 2022 of routine screening results for antibodies to the human immunodeficiency virus (HIV) among members of the active and reserve components of the U.S. Armed Forces. During the full 5 and 1/2-year surveillance period, the HIV seropositivity rates for active component service members were 0.21 positives per 1,000 members of the Army, 0.24 for the Navy, 0.16 for the Marine Corps, and 0.14 for the Air Force. Among reserve service members the rates were 0.34 per 1,000 members of the Army reserve, 0.26 for the Navy reserve, 0.19 for the Marine Corps reserve, and 0.19 for the Air Force reserve. For members of the National Guard, the rates were 0.28 per 1,000 members of the Army Guard and 0.09 for the Air Force Guard. Across active and reserve components of all services, seropositivity rates continued to be higher among male than female service members.
What are the new findings?
From January 2017 through June 2022, the rates of HIV test positivity among uniformed personnel (active component, Guard, and reserve) remained relatively stable. Rates among female service members have remained very low compared to those of male service members.
What is the impact on readiness and force health protection?
For over 30 years, the routine screening for antibodies to HIV has enabled the U.S. military to provide adequate and timely medical care to infected service members, counseling to prevent unwitting transmission, and protection of the battlefield blood supply.
Background
Since acquired immunodeficiency syndrome (AIDS) was first recognized as a distinct clinical entity in 1981,1 its spread has had major impacts on the health of populations and health care systems worldwide. Human immunodeficiency virus type 1 (HIV-1) was identified as the cause of AIDS in 1983. For more than 30 years, the U.S. military has conducted routine screening for antibodies to HIV-1 to enable adequate and timely medical evaluations, treatment, and counseling; to prevent unwitting transmission; and to protect the battlefield blood supply.2,3
As part of the U.S. military’s total-force HIV screening program, civilian applicants for military service are screened for antibodies to HIV during pre-accession medical examinations. Since 1986, all members of the active and reserve components of the U.S. Armed Forces have been periodically screened to detect newly acquired HIV infections. In 2004, the Department of Defense (DOD) set a standard testing interval of 2 years for all service members.4,5 In addition, all military personnel are typically screened for HIV infection before deployment, upon return from deployment, and after having received a diagnosis of various other conditions, such as a sexually transmitted infection.5 Routine HIV screenings are usually performed during the periodic health assessment, an annual evaluation of a service member’s medical readiness status. Service members who are infected with HIV receive clinical assessments, treatments, and counseling.2,3
Before 2009, all of the aforementioned screening programs used laboratory techniques that detected only HIV-1-type infections. Starting in 2009, all programs adopted methods that allowed the detection of antibodies to both major HIV types (i.e., HIV-1 and HIV-2). Although HIV-2 infection is rare in the U.S., it is much more prevalent in other parts of the world where service members may be required to serve. To provide for the change in laboratory methods in the past and for the prospect of future detections of HIV-2 infection in the services’ screening programs, this report will hereafter refer to the target of the screening programs as simply “HIV” without specifying the types.
Infection with HIV has historically been medically disqualifying for entry into U.S. military service. Additionally, active service members were restricted from deploying and were unable to be commissioned as officers if they tested positive for HIV.6,7 However, in light of significant advances in the diagnosis, treatment, and prevention of HIV, the DOD changed its policy in June 2022 such that individuals living with HIV who are symptomatic and have an undetectable viral load will not have restrictions applied to their deployability or ability to be commissioned.8
This report summarizes numbers and trends of newly identified HIV-antibody seropositive cases among members of the active and reserve components of the U.S. Armed Forces from 1 January 2017 through 30 June 2022. Summaries of the results of routine screening for antibodies to HIV among civilian applicants before 2021 and active and reserve component members of the U.S. military since 1990 are available at www.health.mil/MSMRArchives.
Methods
The surveillance period was 1 January 2017 through 30 June 2022. The surveillance population included all individuals who were screened for antibodies to HIV while serving in the active or reserve component of the Army, Navy, Air Force, or Marine Corps during the surveillance period.
All individuals who were tested and all first-time detections of antibodies to HIV through U.S. military medical testing programs were ascertained by matching specimen numbers and serologic test results using unique personal identifiers. All results were accessed from records routinely maintained in the Defense Medical Surveillance System (DMSS). Previous Medical Surveillance Monthly Reports (MSMR) presented HIV screening results for civilian applicants for military service. However, these data are no longer available in the DMSS, as the U.S. Military Entrance Processing Command (MEPCOM) stopped providing data to the DMSS after calendar year 2020.
An incident case of HIV-antibody seropositivity was defined as an individual with positive HIV test results on 2 different, serial specimens. For the sake of this report, individuals who had just 1 positive result but had not yet been tested a second time were counted as positive. Annual rates of HIV seropositivity among service members were calculated by dividing the number of incident cases of HIV-antibody seropositivity during each calendar year by the number of individuals in each component of each service branch who were tested at least once during the relevant calendar year.
Results
Overall
From January 2021 through June 2022, almost 2 million service members (active component, Guard, and reserve) were tested for antibodies to HIV, and 433 were identified as HIV-antibody positive (seropositivity: 0.22 per 1,000 tested) (data not shown). Between 2017 and 2021, annual seropositivity rates fluctuated between a low of 0.19 per 1,000 tested in 2020 and 2022 and a high of 0.23 per 1,000 tested in 2017, 2019, and 2021. Of the 1,581 service members diagnosed with HIV infections since 2017, a total of 981 (62.0%) were still in military service in 2022.
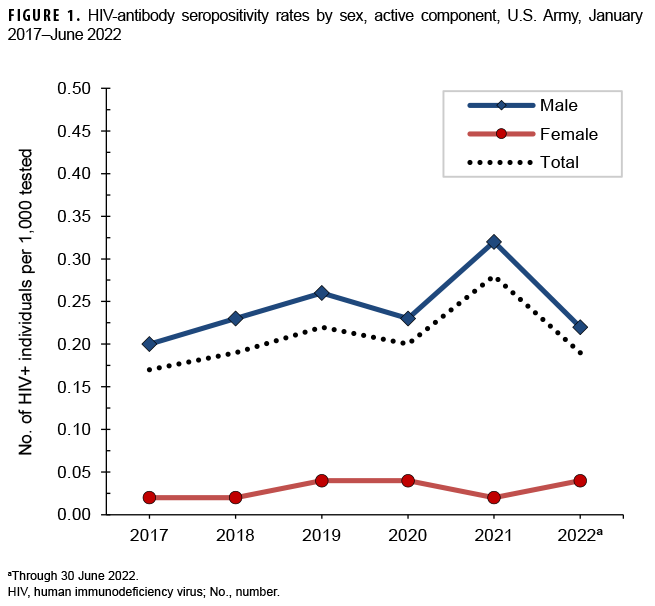
U.S. Army
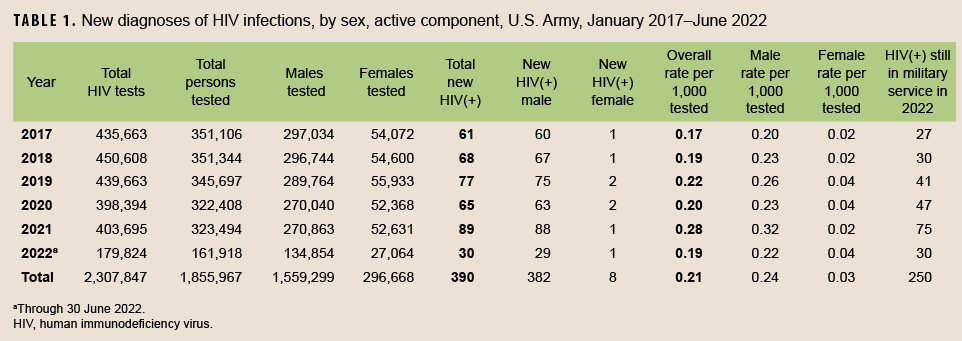
Active component
From January 2021 through June 2022, a total of 485,412 soldiers in the active component of the U.S. Army were tested for antibodies to HIV, and 119 soldiers were identified as HIV-antibody positive (seropositivity: 0.25 per 1,000 soldiers tested) (Table 1). During the surveillance period, annual seropositivity rates fluctuated between a low of 0.17 per 1,000 tested in 2017 and a high of 0.28 per 1,000 tested in 2021 (Table 1, Figure 1). Annual seropositivity rates for male active component soldiers were considerably higher than those of female active component soldiers (Figure 1). During 2021, on average, 1 new HIV infection was detected among active component soldiers per 4,536 screening tests (Table 1). Of the 390 active component soldiers diagnosed with HIV infections since 2017, a total of 250 (64.1%) were still in military service in 2022.
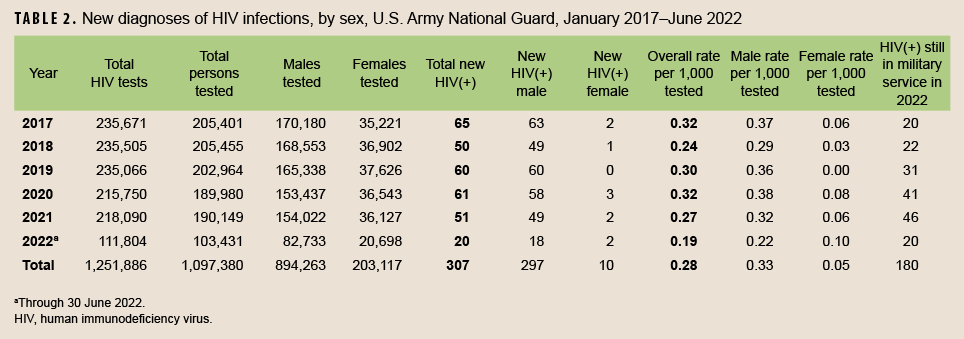
Army National Guard
From January 2021 through June 2022, a total of 293,580 members of the U.S. Army National Guard were tested for antibodies to HIV, and 71 soldiers were identified as HIV-antibody positive (seropositivity: 0.24 per 1,000 soldiers tested) (Table 2). Among Army National Guard soldiers, annual seropositivity rates decreased from 2017 to 2018 (seropositivity rates: 0.32 and 0.24 per 1,000 soldiers tested, respectively), increased in 2019 (0.30 per 1,000 tested) and 2020 (0.32 per 1,000 tested), and then decreased in 2021 (0.27 per 1,000 tested) and during the first 6 months of 2022 (0.19 per 1,000 tested). On average, during 2021, 1 new HIV infection was detected among Army National Guard soldiers per 4,276 screening tests. Of the 307 National Guard soldiers who tested positive for HIV since 2017, a total of 180 (58.6%) were still in military service in 2022.
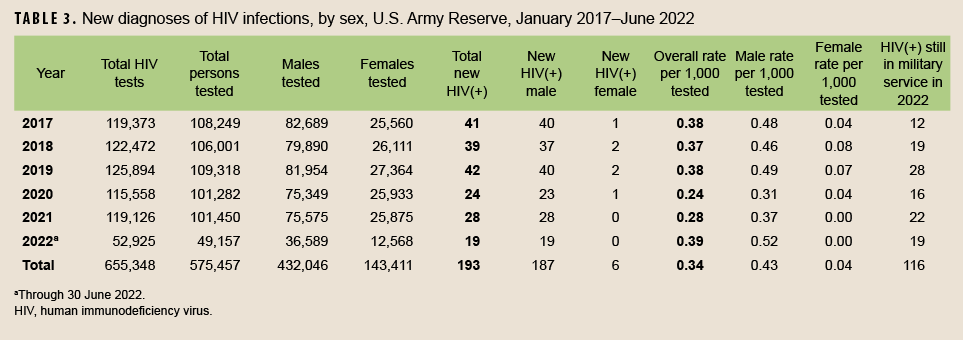
Army Reserve
From January 2021 through June 2022, a total of 150,607 members of the U.S. Army Reserve were tested for antibodies to HIV, and 47 soldiers were identified as HIV-antibody positive (seropositivity: 0.31 per 1,000 soldiers tested) (Table 3). Among Army reservists during the surveillance period, seropositivity rates remained stable between 2017 and 2019 at 0.38 per 1,000 tested. This was followed by a considerable decrease in seropositivity rates in 2020 (0.24 per 1,000 tested), and an increase in 2021 (0.28 per 1,000 tested) and in the first 6 months of 2022 (0.39 per 1,000 tested). During 2021, on average, 1 new HIV infection was detected among Army reservists per 4,255 screening tests (Table 3). Of the 193 Army reservists diagnosed with HIV infections since 2017, a total of 116 (60.1%) were still in military service in 2022.
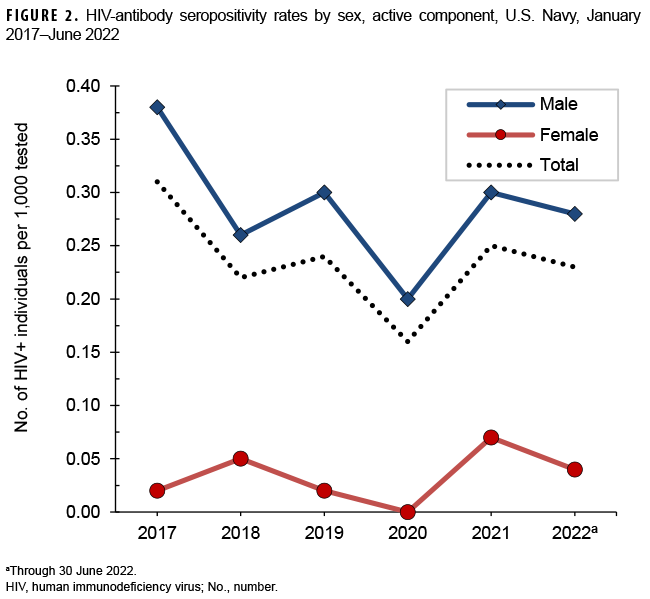
U.S. Navy
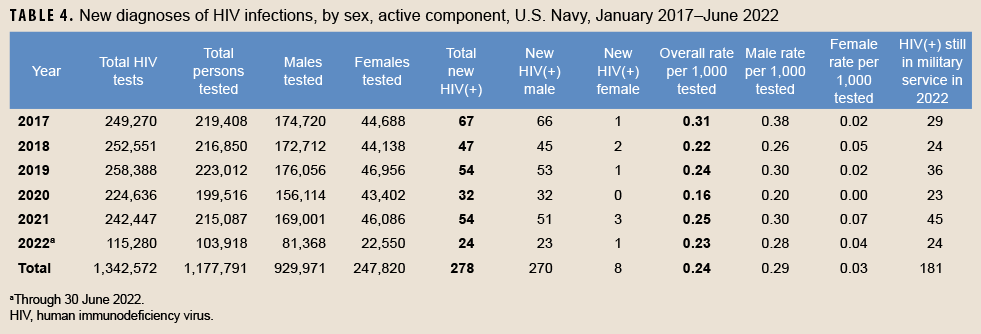
Active component
From January 2021 through June 2022, a total of 319,005 active component members of the U.S. Navy were tested for antibodies to HIV, and 78 sailors were identified as HIV-antibody positive (seropositivity: 0.24 per 1,000 sailors tested) (Table 4). Among tested male active component sailors, full-year annual HIV-antibody seropositivity rates decreased 47.4% between 2017 and 2020 (Figure 2). Annual seropositivity rates increased in 2021 and decreased again in the first 6 months of 2022. During each year of the surveillance period, only 0 to 3 female sailors tested positive. During 2021, on average, 1 new HIV infection was detected among active component sailors per 4,490 screening tests (Table 4). Of the 278 active component sailors who tested positive for HIV since 2017, a total of 181 (65.1%) were still in military service in 2022.
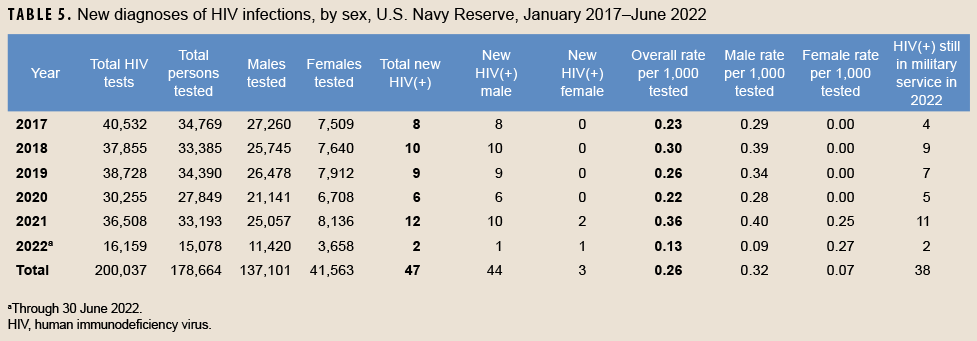
Navy Reserve
From January 2021 through June 2022, a total of 48,271 members of the U.S. Navy Reserve were tested for antibodies to HIV, and 14 sailors were identified as HIV-antibody positive (seropositivity: 0.29 per 1,000 sailors tested) (Table 5). The HIV-antibody seropositivity rates among Navy reservists since 2017 peaked in 2021 (seropositivity rates: 0.36 per 1,000 sailors tested). Between 2008 and 2020, no female Navy reservist was detected with antibodies to HIV during routine testing (data not shown). However, 2 female Navy reservists tested positive in 2021 and 1 tested positive in the first 6 months of 2022. On average, during 2021, 1 new HIV infection was detected among Navy reservists per 3,042 screening tests (Table 5). Of the 47 reserve component sailors diagnosed with HIV infections since 2017, a total of 38 (80.9%) were still in military service in 2022.
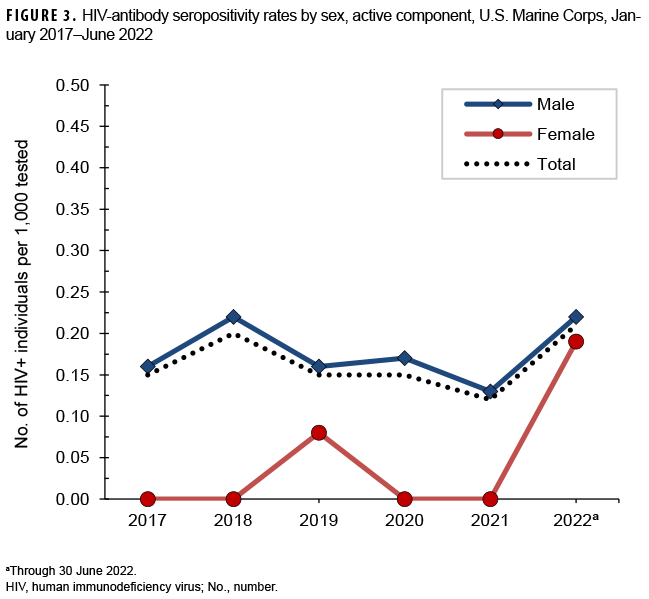
U.S. Marine Corps
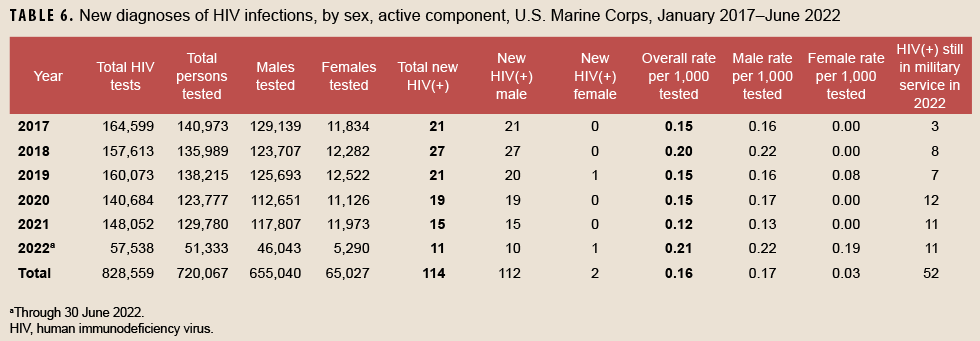
Active component
From January 2021 through June 2022, a total of 181,113 members of the active component of the U.S. Marine Corps were tested for antibodies to HIV, and 26 Marines were identified as HIV-antibody positive (seropositivity: 0.14 per 1,000 Marines tested) (Table 6). From January 2017 through June 2022, seropositivity rates of antibodies to HIV remained relatively low and stable among routinely tested Marines (Figure 3). During 2021, on average, 1 new HIV infection was detected among active component Marines per 9,870 screening tests (Table 6). Of the 114 active component Marines diagnosed with HIV infections since 2017, a total of 52 (45.6%) were still in military service in 2022.
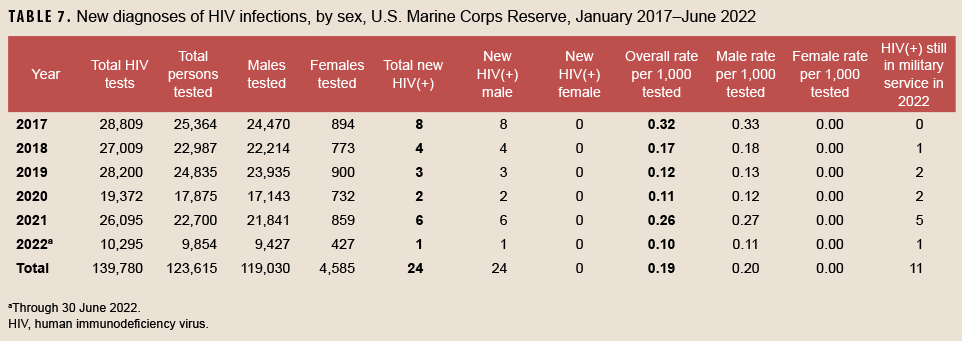
Marine Corps Reserve
From January 2021 through June 2022, a total of 32,554 members of the U.S. Marine Corps Reserve were tested for antibodies to HIV, and 7 Marine Corps reservists were identified as HIV-antibody positive (seropositivity: 0.22 per 1,000 Marines tested) (Table 7). During the surveillance period, seropositivity rates among Marine Corps were highest at 0.32 per 1,000 tested in 2017 and at 0.26 per 1,000 tested in 2021. Seropositivity rates reached a low in 2020 at 0.11 per 1,000 tested. Of note, only 1 female Marine Corps reservist tested positive for antibodies to HIV during routine screening in 2015; none were detected during 1990–2014 or during 2016–2022 (through June) (data not shown). During 2021, on average, 1 new HIV infection was detected among Marine Corps reservists per 4,349 screening tests (Table 7). Of the 24 Marine Corps reservists diagnosed with HIV infection since 2017, a total of 11 (45.8%) were still in military service in 2022.
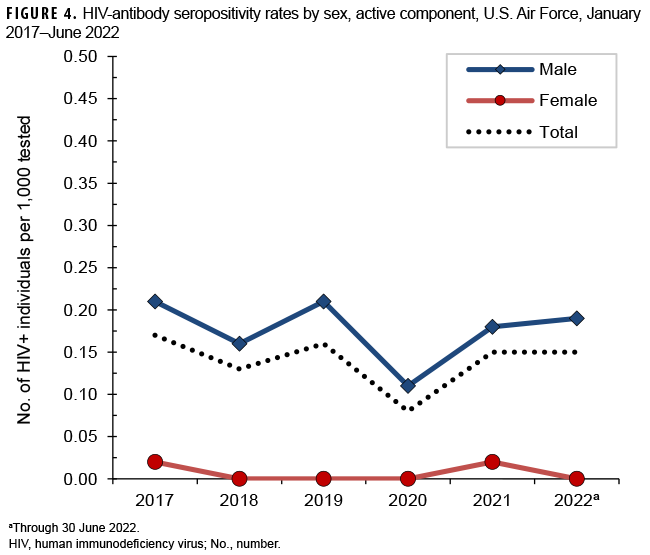
U.S. Air Force
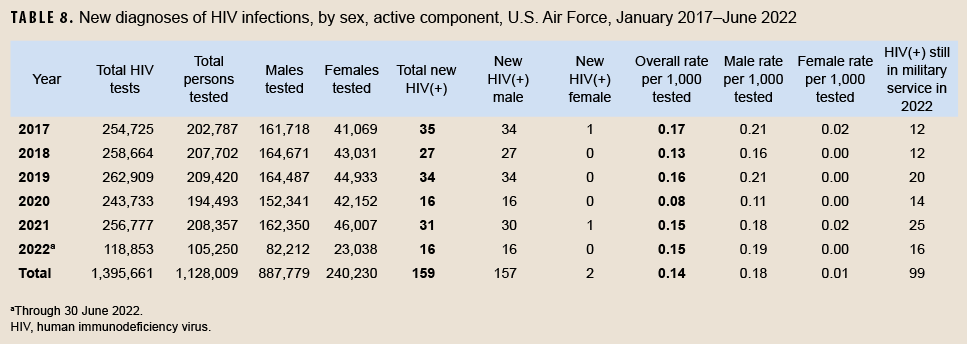
Active component
From January 2021 through June 2022, a total of 313,607 active component members of the U.S. Air Force were tested for antibodies to HIV, and 47 Air Force members were diagnosed with HIV infections (seropositivity: 0.15 per 1,000 Air Force members tested) (Table 8). During the surveillance period, seropositivity rates among male members ranged from a high of 0.21 per 1,000 tested in 2017 and 2019 to a low of 0.11 per 1,000 tested in 2020. (Figure 4). Among female Air Force members during the surveillance period, annual seropositivity rates remained relatively low and stable. During 2021, on average, 1 new HIV infection was detected among active component Air Force members per 8,283 screening tests (Table 8). Of the 159 active component Air Force members diagnosed with HIV infections since 2017, 99 (62.3%) were still in military service in 2022.
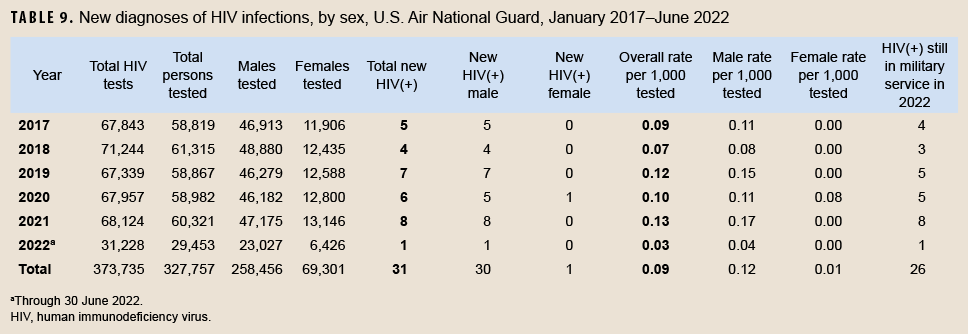
Air National Guard
From January 2021 through June 2022, a total of 89,774 members of the Air National Guard were tested for antibodies to HIV, and 9 Air National Guard members were diagnosed with HIV infections (seropositivity: 0.10 per 1,000 Air National Guard members tested) (Table 9). In 2020, 1 female Air National Guard member was detected with antibodies to HIV, the first since 2010 (data not shown). During 2021, on average, 1 new HIV infection was detected among Air National Guard members per 8,516 screening tests (Table 9). Of the 31 Air National Guard members diagnosed with HIV infections since 2017, 26 (83.9%) were still in military service in 2022.
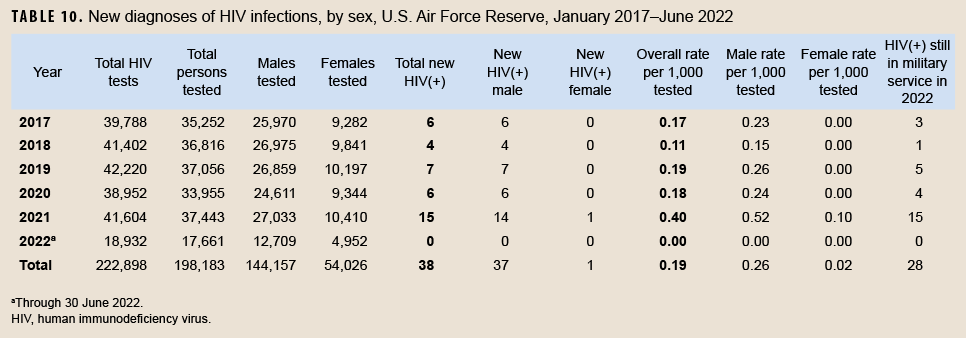
Air Force Reserve
From January 2021 through June 2022, a total of 55,104 members of the Air Force Reserve were tested for antibodies to HIV, and 15 Air Force reservists were diagnosed with HIV infections (seropositivity: 0.27 per 1,000 airmen tested) (Table 10). During 2021, on average, 1 new HIV infection was detected among Air Force reservists per 2,774 screening tests (Table 10). Of the 38 Air Force reservists diagnosed with HIV infections since 2017, 28 (73.7%) were still in military service in 2022.
Editorial Comment
The U.S. military has conducted routine screening for antibodies to HIV among all civilian applicants for service and all active and reserve component members of the services for more than 30 years.2-5 Results of U.S. military HIV-antibody testing programs have been summarized in the MSMR for more than 2 decades.9 Results of HIV screening among civilian applicants for service were last summarized in the September 2021 issue of the MSMR.10
This report documents that full-year HIV-antibody seropositivity rates among members of the active components ranged from 0.08 per 1,000 tested (Air Force, 2020) to 0.31 per 1,000 tested (Navy, 2017). Full-year seropositivity rates among the reserve/Guard components fluctuated between 0.07 per 1,000 tested (Air National Guard, 2018) and 0.40 per 1,000 tested (Air Force Reserve, 2021); the greatest variations in full-year seropositivity rates were observed among Marine Corps reservists. Full year seropositivity rates peaked in 2021 for active component service members of the Army, in 2017 for the Navy, in 2018 for the Marine Corps, and in 2017 for the Air Force. Among reserve and National Guard members, full year seropositivity peaked in 2021 for the Air Force National Guard, in 2021 for the Air Force reserve, in 2017 for the Marine Corps reserve, in 2021 for the Navy reserve, in 2017 and 2019 for the Army reserve, and in 2017 and 2020 for the Army National Guard. Overall (January 2017–June 2022) HIV-antibody seropositivity rates were highest among Army reservists, Army National Guard members, and Navy reservists and lowest among Air National Guard members, Marine Corps active component members, and Air Force active component members. Across active and reserve components of all services, seropositivity rates continued to be higher among male than female service members.
There are several limitations that should be considered when interpreting the results of the current analysis. For example, because of the frequency of screening in the military (as an applicant, routinely every 2 years, and before and after overseas deployments), routine screening now detects relatively recently acquired HIV infections (i.e., infections acquired since the most recent negative test of each affected individual). As such, annual HIV-antibody seropositivity rates obtained during routine screening of military populations are reflective of, but are not direct unbiased estimates of, incidence rates and acquisition trends of HIV infections among military members.
In summary, the U.S. military has conducted comprehensive HIV prevention, education, counseling, and treatment programs for more than 30 years. Since the beginning of these programs, routine screening of all civilian applicants for service and routine periodic testing of all active and reserve component members of the services have been fundamental components of the military’s HIV control and clinical management efforts.11 Summaries of results of screening programs such as those in this report provide insights into the current status and trends of the impact of HIV in various U.S. military populations.
Given the consistently low detection rates associated with routine screening of the entire military force, future studies may be undertaken to describe healthcare seeking behaviors among those service members most at risk of subsequent infection. Results of such studies might identify opportunities for indications-based testing in lieu of universal testing.
References
- Centers for Disease Control and Prevention. Kaposi’s sarcoma and Pneumocystis pneumonia among homosexual men—New York City and California. MMWR Morb Mortal Wkly Rep. 1981;30(25):305–308.
- Tramont EC, Burke DS. AIDS/HIV in the U.S. military. Vaccine. 1993;11(5):529–533.
- Brown AE, Brundage JF, Tomlinson JP, Burke DS. The U.S. Army HIV testing program: the first decade. Mil Med. 1996;161(2):117–122.
- Office of the Assistant Secretary of Defense. Health Affairs Policy Memorandum—Human Immunodeficiency Virus Interval Testing. HA Policy 04-007. 29 March 2004.
- Office of the Under Secretary of Defense for Personnel and Readiness. Department of Defense Instruction 6485.01. Human Immunodeficiency Virus (HIV) in Military Service Members. 7 June 2013.
- Office of the Under Secretary of Defense for Personnel and Readiness. Department of Defense Instruction 6130.03, Medical Standards for Appointment, Enlistment, or Induction in the Military Services. 6 May 2018.
- Office of the Under Secretary of Defense for Personnel and Readiness. Department of Defense Instruction 1332.45, Retention Determinations for Non-Deployable Service Members. 30 July 2018.
- Secretary of Defense Memorandum for Senior Pentagon Leadership, Commanders of the Combatant Commands, Defense Agency and DoD Field Activity Directors. Policy Regarding Human Immunodeficiency Virus-Positive Personnel Within the Armed Forces. June 6, 2022.
- Army Medical Surveillance Activity. Supplement: HIV-1 in the Army. MSMR. 1995;1(3):12–15.
- Armed Forces Health Surveillance Division. Update: Routine screening for antibodies to human immunodeficiency virus, civilian applicants for U.S. military service and U.S. Armed Forces, active and reserve components, January 2016–June 2021. MSMR. 2021;28(9):18–27.
- Okulicz JF, Beckett CG, Blaylock JM, et al. Review of the U.S. military’s human immunodeficiency virus program: a legacy of progress and a future of promise. MSMR. 2017;24(9):2–7.