The Department of Defense (DOD) publishes annual hospitalization trends for active component members of the U.S. Armed Forces. These published reports describe demographics, duration of stay, and hospitalization rates by disease categories.1 Due to missing data, however, these reports have not included hospitalization data for U.S. Coast Guard (USCG) service members since 2015.2
The Coast Guard is a military service within the Department of Homeland Security (DHS) that provides limited primary care for its personnel through 43 outpatient clinics but does not maintain inpatient facilities.3 USCG service members are eligible for health care through DOD’s TRICARE Prime program, including Click to closeDirect CareDirect care refers to military hospitals and clinics, also known as “military treatment facilities” and “MTFs.”direct care at military hospitals and Click to closePurchased CareThe TRICARE Health Program is often referred to as purchased care. It is the services we “purchase” through the managed care support contracts.purchased care through TRICARE networks of civilian providers.
This report presents USCG hospitalization data for fiscal year (FY) 2021 to explore the extent of data completeness. The second aim is to describe utilization differences by comparing previously published DOD active component hospitalization data for the calendar year 2021.1
Methods
This report utilizes USCG hospitalization data from the Military Health System Management and Reporting tool, also known as MHS MART or M2, which includes both non-military hospitals covered by TRICARE (purchased care) and DOD military hospitals (direct care). The study population consisted of all USCG members on active status for at least 30 days between October 1, 2020 and September 30, 2021 that produced an inpatient data record from a hospital stay and discharge date before October 1, 2021. Home health agency admissions, observational stays, and inpatient records generated from USCG Defense Medical Information System (DMIS) IDs were assumed to be observational stays and were excluded from this study.
Diagnostic categories were based on the primary condition for hospitalization4 and classified using the letter and first 2 numeric digits of the corresponding International Classification of Diseases 10th Revision (ICD-10) code. The fourth ICD-10 digit was evaluated to more specifically quantify the 10 most frequent primary causes of hospitalization. Rate calculations per 1,000 personnel utilized USCG workforce data from October 2020, which indicated a total force strength of 40,558.5 Category-specific rates were not calculated for hospitalization counts under 20 due to estimate instability.6 The length of stay was calculated as the difference (in days) between end date of care and start date of care. All descriptive statistics were calculated using Excel 2018 (Microsoft Corp).
The USCG Commandant Institutional Review Board determined this work relates to public health surveillance and monitoring for programmatic improvement and does not constitute research.
Results
In FY 2021, the estimated USCG active duty service member yearly hospitalization rate (28.8 per 1,000 persons) was substantially lower than the rate reported for the DOD active component (48.0 per 1,000 person-years [p-yrs]) in calendar year (CY) 2021 (Table 1). While most hospitalizations among USCG service members occurred at non-military hospitals (84.3%), active component DOD service members primarily received care at military hospitals (only 36.6% were hospitalized at non-military hospitals during CY 2021).1 In both populations, the median duration of hospital stay (for all causes) was 3 days, with the maximum median duration of stay (USCG: 7 days; DOD: 6 days) observed for mental health hospitalizations (data not shown).1
The estimated rates of hospitalization for all major diagnostic categories were lower among USCG active duty service members, with the exception of digestive disorder hospitalizations among women. When excluding pregnancy-related hospitalizations, hospitalization rates remained higher for both USCG and DOD women, compared to their male counterparts (33.5% and 43.6% higher, respectively). The 4 most frequent major diagnostic categories for hospitalization included pregnancy and delivery, mental health conditions, injury/poisoning, and digestive disorders, as shown in Table 1. 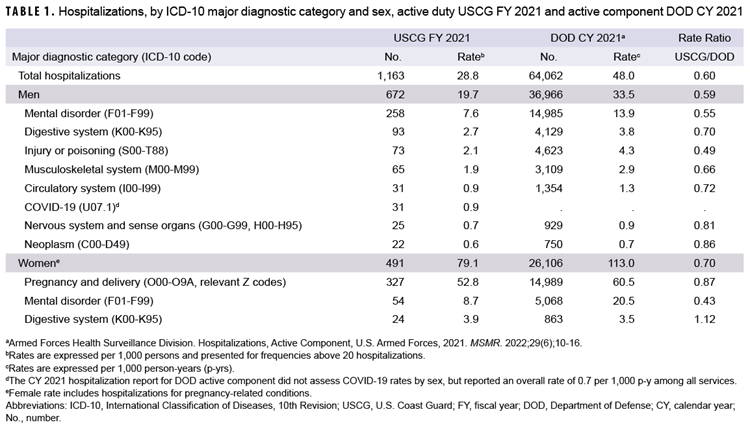
Table 2 depicts the 10 most frequent causes assessed through the fourth digit ICD-10 code. 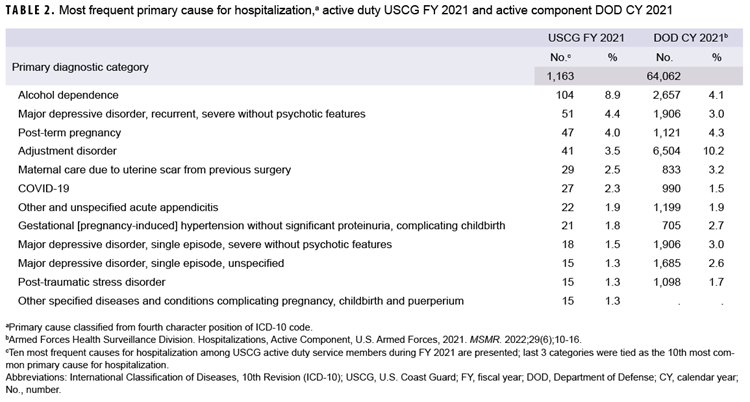
While adjustment disorders accounted for the most frequent primary cause of mental health disorder hospitalizations in DOD active component service members (10.2%), alcohol dependence was the most common diagnosis among hospitalized USCG active duty service members (8.9%).
Discussion
The 40% lower observed rate of hospitalization among USCG active duty service members compared to the DOD active component indicates that concerns raised in 2015 regarding incomplete capture of USCG hospitalization data have not been completely addressed.2 In relatively large populations comparable in age, gender, medical screening, and work status, there is an expectation that hospitalization rates will be very similar. Despite this possibility of incomplete data, the FY 2021 USCG active duty service member population shares specific characteristics with CY 2021 data1 from other military services. Observed similarities include common major diagnostic categories (mental health, pregnancy-related, injury/poisoning, and digestive disorders); concordance among 8 of the 10 most common primary causes for hospitalization; comparable durations of stay; and increased non-pregnancy-related hospitalization rates among women. These similarities imply that the hospitalization data obtained through M2 are likely a representative sample of the full dataset.
When excluding pregnancy-related hospitalizations, mental health conditions represent the most common major diagnostic category among both men and women. Six separate primary diagnostic categories within this major category accounted for 21.0% of all hospitalizations among USCG active duty service members.
This analysis is subject to additional limitations beyond the potential of data incompleteness. First, this paper calculated USCG hospitalization rates differently from those reported for the DOD, which utilized the total number of days of active component service during which a service member was considered at risk for a given condition. Given the minor change in USCG active duty end strength over the study period (40,421 on October 1, 2020 and 40,487 on October 1, 2021), however, the difference in rate calculation methodology would not likely significantly affect the results. Second, as this analysis is based on primary (first-listed) discharge diagnoses only, it does not account for multiple underlying conditions that may have contributed to hospital stays.
An exploration of the sources and potential solutions for this data incompleteness would be an important next step for accurately capturing USCG hospital utilization. An analysis of hospitalizations by type of care (direct vs. purchased) as well as facility for a longitudinal period may better define areas of incomplete data capture. Future analyses should also explore additional covariates, including age, to align rate calculation methods for facilitating comparability of hospitalization data with other military services.
References
- Armed Forces Health Surveillance Division. Hospitalizations, active component, U.S. Armed Forces, 2021. MSMR. 2022;29(6):10-16.
- Armed Forces Health Surveillance Branch. Hospitalizations among members of the active component, U.S. Armed Forces, 2015. MSMR. 2016;23(4):8-16.
- U.S. Government Accountability Office. Coast Guard Health Care: Improvements Needed for Determining Staffing Needs and Monitoring Access to Care. Accessed February 22, 2022. https://www.gao.gov/products/gao-22-105152
- MDR, M2, ICDs Functional References and Specifications. Military Health System and Defense Health Agency. Updated January 17, 2023. Accessed February 1, 2023. https://www.health.mil/Military-Health-Topics/Technology/Support-Areas/MDR-M2-ICD-Functional-References-and-Specification-Documents
- Department of Defense, Office of the Deputy Assistant Secretary of Defense for Military Community and Family Policy. 2020 Demographics Profile of the Military Community. Accessed February 1, 2023. https://www.militaryonesource.mil/data-research-and-statistics/military-community-demographics/2020-demographics-profile
- New York State Department of Health. Rates Based on Small Numbers-Statistics Teaching Tools. Updated April 1999. Accessed February 1, 2023. https://www.health.ny.gov/diseases/chronic/ratesmall.htm