This report documents the frequencies, rates, trends, and distributions of hospitalization among active component members of the U.S. Army, Navy, Air Force, and Marine Corps during calendar year 2022. Summaries are based on standardized hospitalization records at U.S. military and non-military (reimbursed through the Military Health System) medical facilities worldwide that are routinely maintained in the Defense Medical Surveillance System. This is the first year that DMSS data were housed and analyzed from the Military Health System Information Platform. Data quality assessments for completeness and timeliness are ongoing during the transition to MIP. Thus, data presented in this report are considered provisional but current as of March 28, 2023.
In this report, primary (first-listed) discharge diagnoses are considered indicative of the main reason for hospitalization. As in previous MSMR reports, summaries are based on the first 3 digits of the International Classification of Diseases, 10th Revision of the primary discharge diagnoses. Hospitalizations not routinely documented by standardized, automated records, e.g., during field training exercises or while shipboard, are not available in a centralized location for health surveillance purposes and are excluded from this report. Incidence rates were calculated per 1,000 p-yrs. Percent change in incidence was calculated using unrounded rates.
What are the new findings?
The provisional estimate of the hospitalization rate in U.S. military and non-military medical facilities in 2022 is 43.9 per 1,000 person-years (p-yrs), the lowest rate in 10 years. As in prior years, the majority (57.5%) of hospitalizations were associated with primary diagnoses in the categories of mental health disorders and pregnancy-related conditions. Less than 0.5% of total hospitalizations in active component service members in 2022 were attributed to COVID-19, a substantial decrease from 1.5% in 2021.
What is the impact on readiness and force health protection?
As in previous years, mental health disorders, including substance abuse disorders, were associated with the longest median hospital stay (6 days). Moreover, 5% of mental health disorder hospitalizations lasted longer than 30 days. Prolonged hospitalizations, aftercare, and early attrition due to these common disorders can diminish not only individual but unit operational readiness.
Frequencies, rates, and trends
In 2022, 57,009 hospitalizations were recorded for the active component members of the U.S. Army, Navy, Air Force, and Marine Corps (Table 1); 46.4% of these hospitalizations were in non-military facilities (data not shown), compared to 37.7% in 2021.
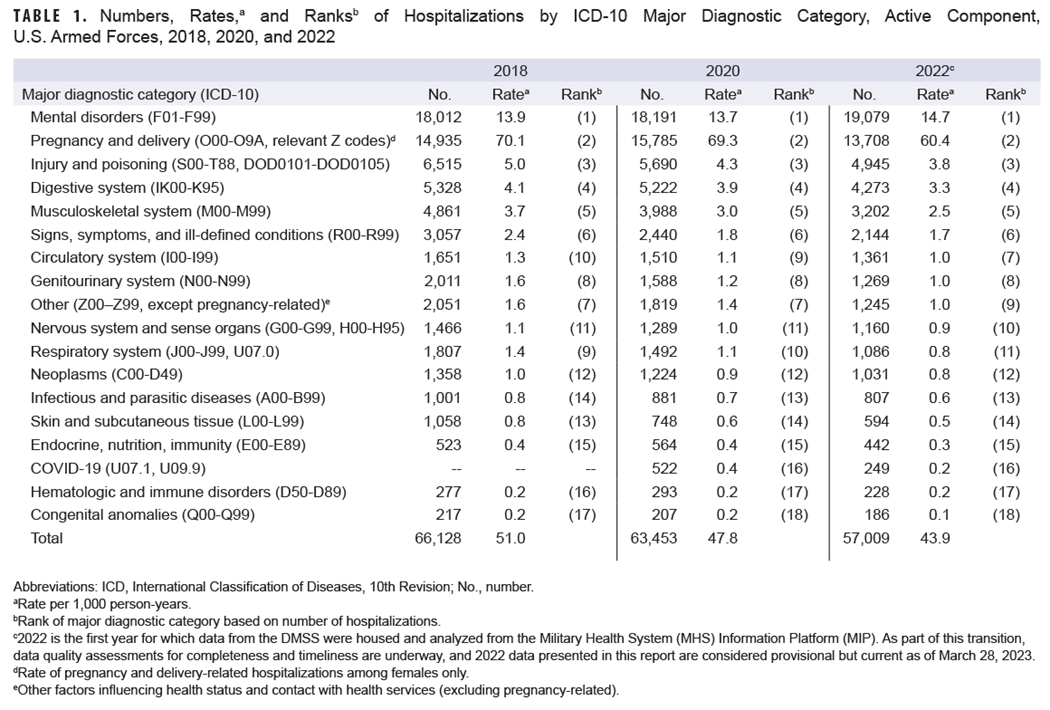
The crude annual hospitalization rate (all causes) in 2022 was 43.9 per 1,000 service member p-yrs (Table 1), the lowest rate from 2013 through 2022, during which rates fell 23.8% (Figure 1).
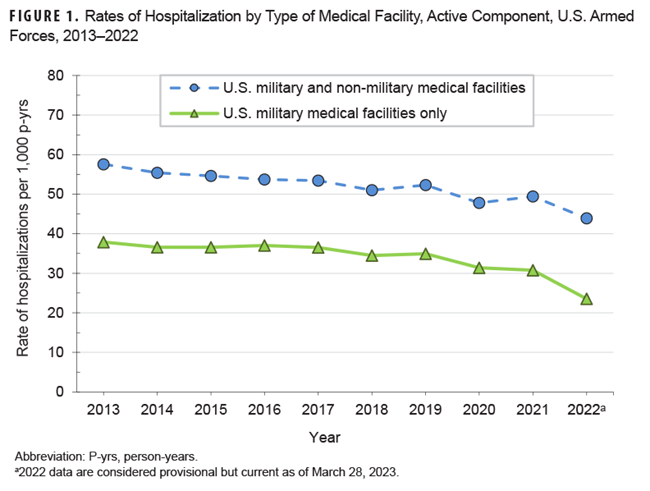
Provisional data indicate that hospitalization rates have declined monotonically over the past 10 years, with the largest rate drop, 12%, within the current reporting period.
Hospitalizations by ICD-10 major diagnostic categories
In 2022, four ICD-10 major diagnostic categories accounted for almost three-quarters (73.7%) of all active component hospitalizations: mental health disorders (33.5%), pregnancy- and delivery-related conditions (24.0%), injury (8.7%), and digestive system disorders (7.5%) (Table 1). Consistent with findings from 2018 and 2020, hospitalizations for mental health disorders in 2022 accounted for more than for any other major diagnostic category; 2009 was the last year in which another diagnostic category (pregnancy- and delivery-related conditions) surpassed hospitalizations for mental health disorders (data not shown). COVID-19 accounted for 0.44% of total hospitalizations in active component service members in 2022, a 70% decline from 1.5% in 2021.
Provisional data indicate that numbers and rates of hospitalizations from 2018 to 2022 decreased for all major diagnostic categories except mental health disorders, which increased slightly (5.7% to 5.9%) (Table 1). The largest decline in hospitalizations from 2018 to 2022 was in the musculoskeletal system and connective tissue diagnostic category (1,659 fewer hospitalizations; 34.1% decrease). The next largest drop in hospitalizations from 2018 to 2022 was in the injury category (1,570 fewer hospitalizations; 24.1% decrease). The largest hospitalization rate declines occurred in the categories of skin and subcutaneous tissue (44.0%), respiratory system (40.0%), other (39.4%), and genitourinary system (37.0%).
The relative proportion of hospitalizations by major diagnostic category was generally stable over the surveillance period (Table 1). COVID-19 was included as a separate diagnostic category in 2020 and ranked 13th in total hospitalizations, but declined to 16th in total visits in 2022.
Hospitalizations, by sex
The hospitalization rate (all causes) among service women in 2022 was more than three times that of service men (101.9 per 1,000 p-yrs and 31.4 per 1,000 p-yrs, respectively). These data are consistent with general U.S. population hospitalization rate trends published in 2022 for women and men aged 18-44 (95 per 1,000 p-yrs and 37 per 1,000 p-yrs respectively).1 Excluding pregnancy and delivery, the rate of hospitalizations among women (41.7 per 1,000 p-yrs) was 32.2% higher than among men (31.6 per 1,000 p-yrs) in 2022 (data not shown). This rate difference was primarily due mental health disorder hospitalizations (female : male rate difference [RD]: 6.6 per 1,000 p-yrs) and genitourinary disorders (RD: 2.0 per 1,000 p-yrs) (data not shown). Excluding pregnancy- and delivery-related conditions, hospitalization rates were relatively similar among men and women for the remaining 15 major diagnostic categories (data not shown).
Relationships between age and hospitalization rates varied by major diagnostic category (Figure 2).
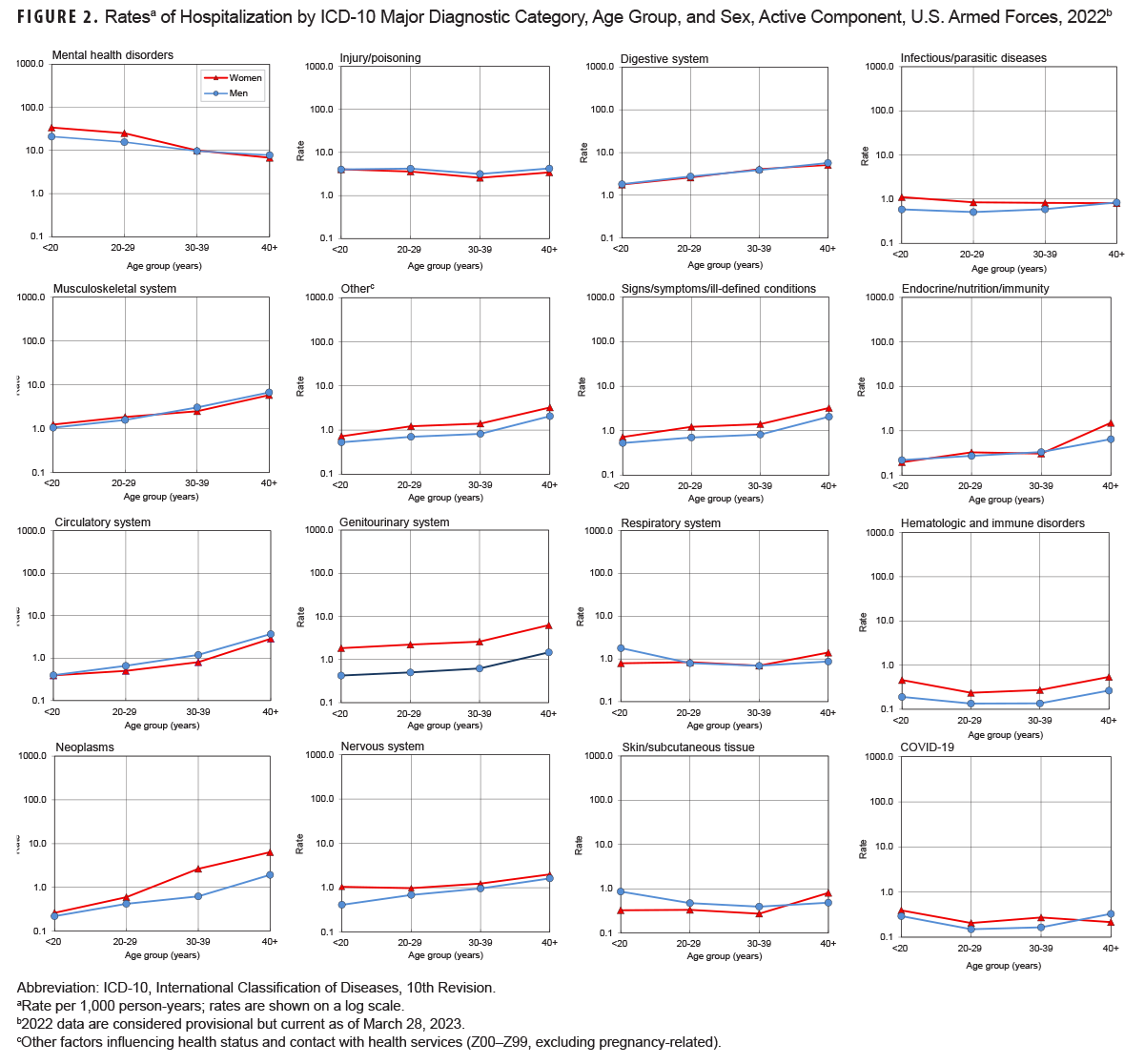
Rates among women in all age groups were consistently higher for several categories: other factors influencing health status and contact with health services; signs/symptoms and other ill-defined conditions; genitourinary system; neoplasms; nervous system; and hematologic and immune disorders. Except in the youngest age group, male rates were higher for the injury and circulatory system categories. Among both sexes, hospitalization rates generally increased with age for neoplasms, musculoskeletal system/connective tissue disorders, digestive system diseases, genitourinary system diseases, circulatory system diseases, other factors influencing health status and contact with health services, and signs/symptoms and other ill-defined conditions. Rates decreased with increasing age for mental health disorders and were relatively stable across all age groups for injury, infectious/parasitic diseases, respiratory system disorders, skin and subcutaneous tissue, hematologic and immune disorders, as well as COVID-19.
Most frequent diagnoses
Adjustment disorders was the most frequent primary discharge diagnosis among both men (n=4,861) and women (n=1,321) (Table 2), accounting for 10.8% of total hospitalizations in 2022.
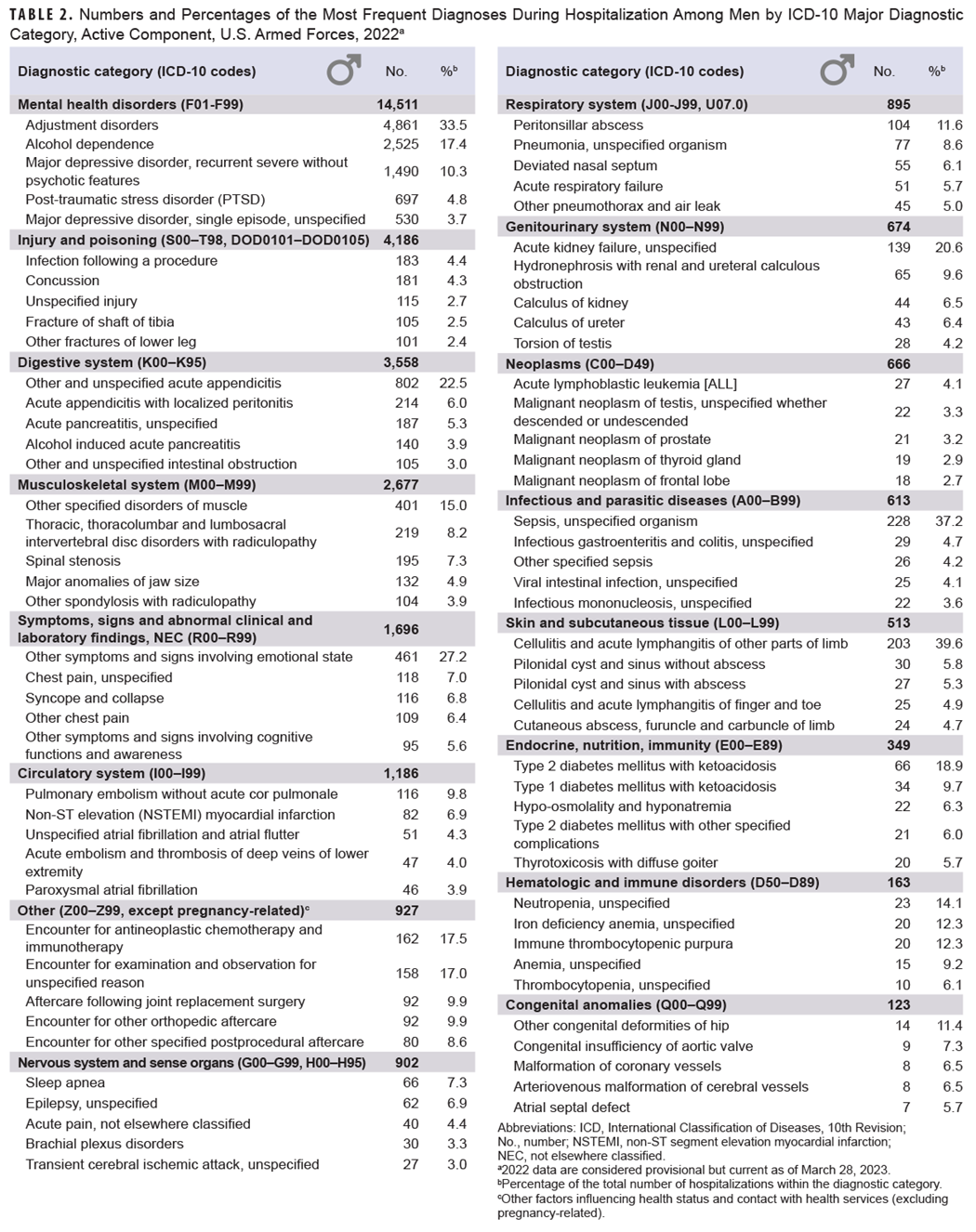
Alcohol dependence (n=2,525), recurrent major depressive disorder (severe without psychotic features) (n=1,490), other and unspecified acute appendicitis (n=802), post-traumatic stress disorder (n=697), and single episode major depressive disorder (unspecified) (n=530) were the next most frequent diagnoses in men (Table 2). Mental health disorder diagnoses accounted for more than two-fifths (42.9 %) of all hospitalizations among men.
For women, pregnancy- and delivery-related conditions constituted the leading major diagnostic category, accounting for almost three-fifths (59.1%) of all female hospitalizations, although adjustment disorders were the most frequent cause when examining ICD-10 diagnoses through the fourth character (Table 3).
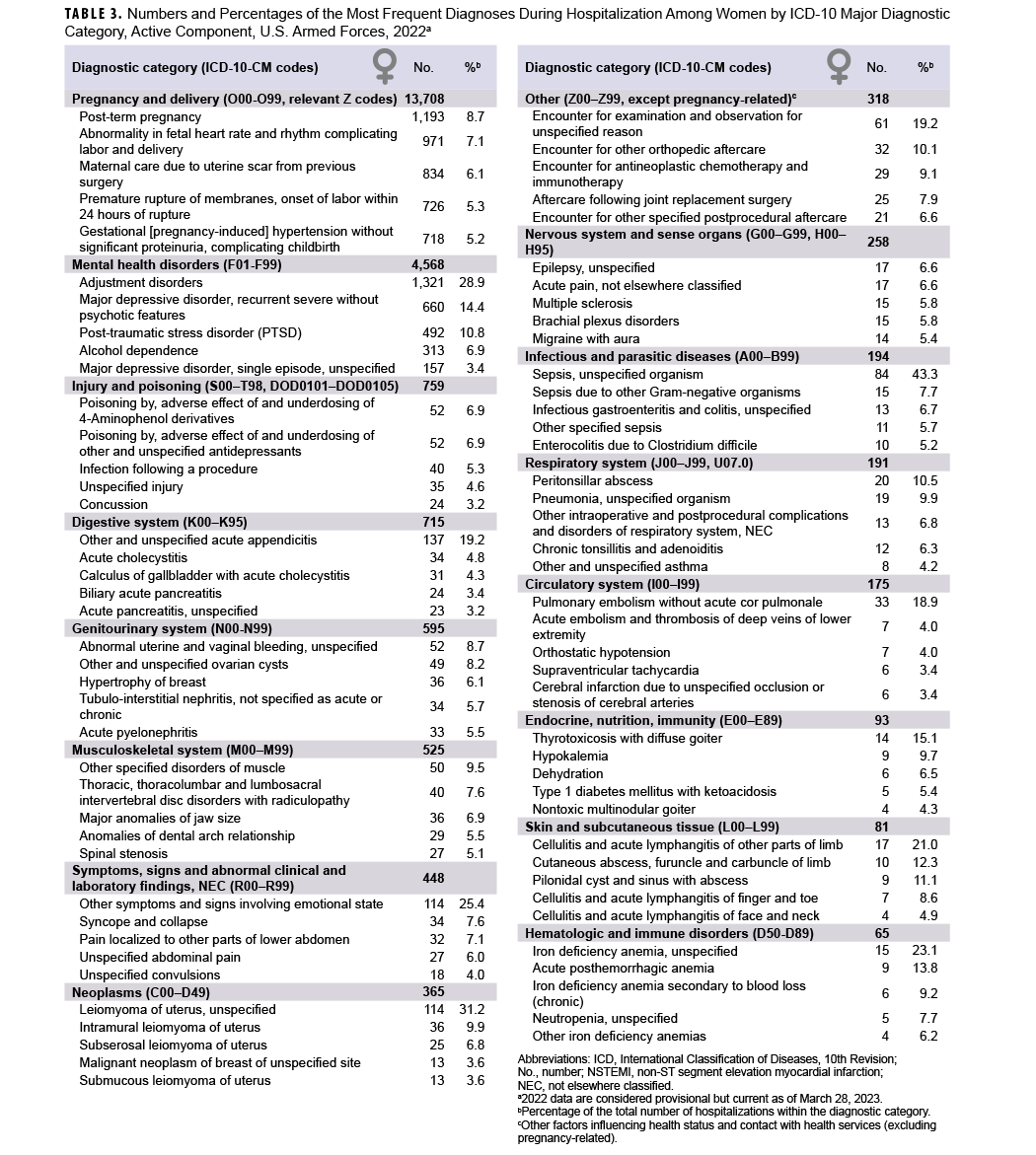
Other leading causes of hospitalization included recurrent major depressive disorder (severe without psychotic features) (n=660), PTSD (n=492), and alcohol dependence (n=313). Mental health disorder diagnoses accounted for about one-fifth (19.7 %) of all hospitalizations among women (Table 3).
Durations of hospitalizations
Hospitalization durations show a highly right-skewed (positive) distribution when charted, with the lower limit equal to one day and a mode of two days. Because length of hospital stay is not normally distributed, the median duration with interquartile range was chosen as the best measure of central tendency. From 2013 to 2022, the median (IQR) duration of hospital stays (all causes) remained stable at three (2-5) days with an increase to four (2-6) days in 2022 (Figure 3).
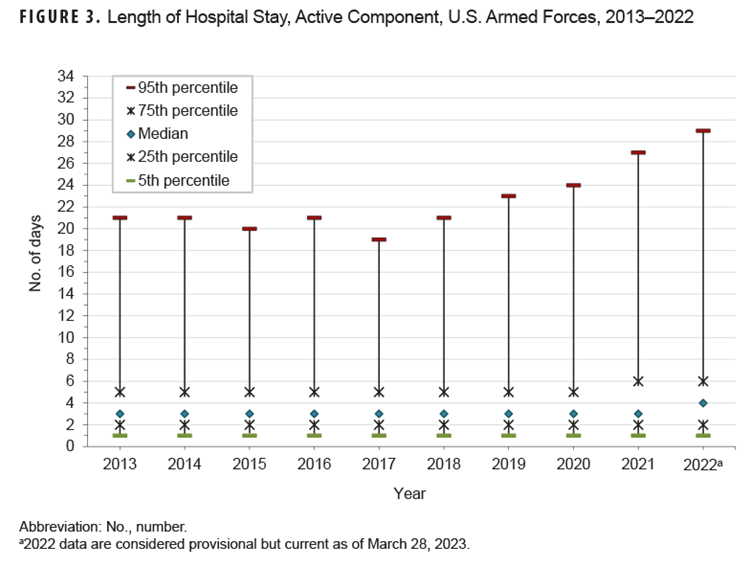
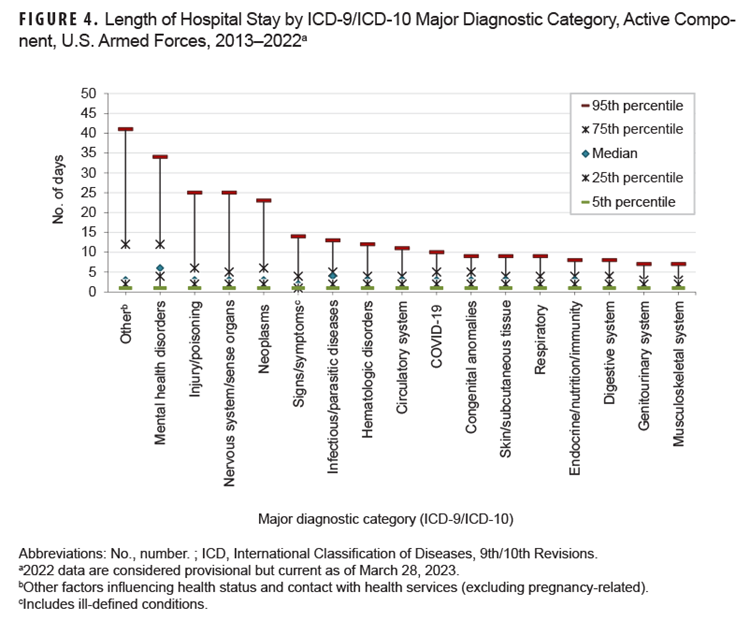
Medians and IQRs of hospitalization durations varied substantially by major diagnostic category. Median lengths of hospitalization varied from two (2-4) days (musculoskeletal system [2-3]; genitourinary system disorders [2-3]; digestive system; respiratory system [2-4]; signs, symptoms, and ill-defined conditions [1-4]) to six days for mental health disorders (4-12). For one half of ICD diagnostic categories, 5% of hospitalizations exceeded 10 days: circulatory system disorders (11 days), hematologic and immune disorders (12 days), signs, symptoms, and ill-defined conditions (14 days), COVID-19 (18 days), neoplasms (23 days), nervous system/sense organ disorders (25 days), injury/poisoning (25 days), mental health disorders (34 days), and other non-pregnancy-related factors influencing health status and contact with health services (primarily orthopedic aftercare and rehabilitation following prior illness or injury) (41 days) (Figure 4).
Hospitalizations, by service
Among Air Force active component members, pregnancy- and delivery-related conditions accounted for more hospitalizations than any other illnesses or injury category, while among active component members of the Army, Navy, and Marine Corps, mental health disorders were the leading cause (Table 4), a pattern observed in recent years.
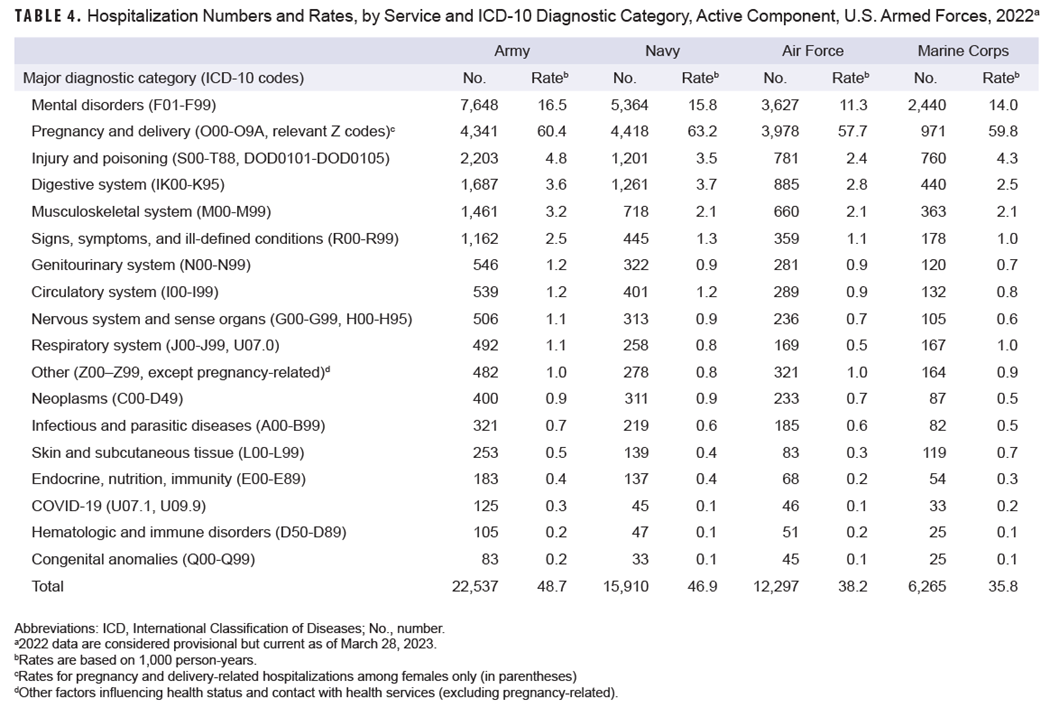
Prior to 2020, pregnancy- and delivery-related conditions were ranked first for both the Navy and Air Force. Among all services the crude hospitalization rate for mental health disorders was highest among active component Army members (16.5 per 1,000 p-yrs).
Injury was the third leading hospitalization category in the Army and Marine Corps, and fourth in the Navy and Air Force. The hospitalization rate for injury was highest for Army (4.8 per 1,000 p-yrs) and Marine Corps members (4.3 per 1,000 p-yrs) and lowest in the Air Force (2.4 per 1,000 p-yrs), a service-ranked distribution observed since 2010.
Discussion
The total hospitalization rate for all causes in both military and non-military medical facilities among active component members in 2022 was the lowest in the past decade. As in past years, in 2022 mental health disorders, pregnancy- and delivery-related conditions, and injury accounted for more than half of all active component hospitalizations. Adjustment disorders, alcohol dependence, depressive disorders, and PTSD were among the leading primary discharge diagnoses for both men and women. The continued decline of hospitalization frequencies and rates in 2022 is attributed to a generalized decline for most major diagnostic categories since 2019, with substantial declines in the musculoskeletal system and injury categories.
Certain limitations should be considered when interpreting these results. The data presented in this report are considered provisional, as ongoing assessments of data completeness in the MHS MIP and any subsequent resolutions may result in changes in trends reported here. This summary is based on primary (first-listed) discharge diagnoses only, but in many hospitalized cases multiple conditions can be present; for example, joint pain (category: musculoskeletal) may be co-listed with an injury (category: injury). In such cases, only the first-listed discharge diagnosis would be accounted in this report, which could underestimate hospitalization rates for common conditions by dividing them among two or more subcategories.
Medical data from July 2017 to October 2019 at sites that had already transitioned to the new MHS electronic health record system, MHS GENESIS, are not available in the DMSS and thus not included in this report—these sites include Naval Hospital Oak Harbor, Naval Hospital Bremerton, Air Force Medical Services Fairchild, and Madigan Army Medical Center. These missing data reduce the true hospitalization rates for that period.
Reference
- National Center for Health Statistics. National Health Interview Survey. Health, United States, 2020-2021. Table HospStay. Accessed June 15, 2023. https://www.cdc.gov/nchs/data/hus/2020-2021/HospStay.pdf