What are the new findings?
The hospitalization rate in 2021 was 48.0 per 1,000 person-years (p-yrs), the second lowest rate of the most recent 10 years. For hospitalizations limited to military facilities, the rate in 2021 was the lowest for the entire period. As in prior years, the majority (71.2%) of hospitalizations were associated with diagnoses in the categories of mental health disorders, pregnancy-related conditions, injury/poisoning, and digestive system disorders.
What is the impact on readiness and force health protection?
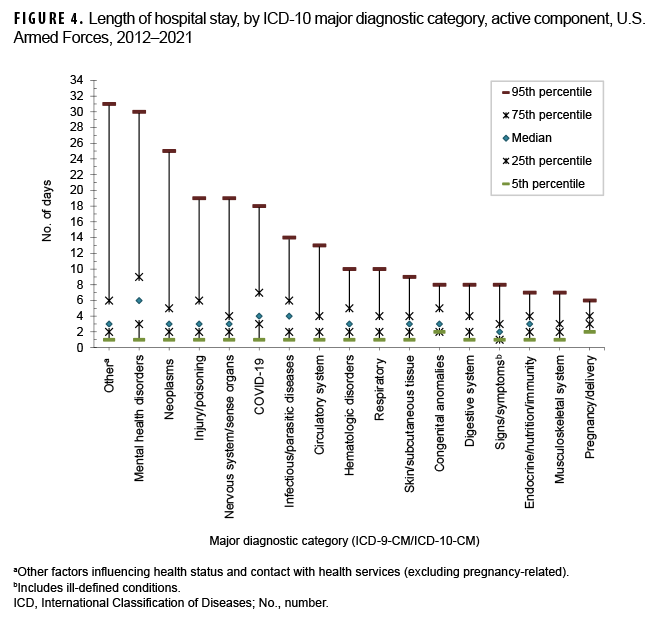
Not only are mental health disorders the most common diagnoses associated with hospitalizations, they are associated with the longest median hospital stay (6 days). Moreover, 5% of hospitalizations for mental health disorders had durations of stay greater than 30 days. Prolonged hospitalizations, subsequent aftercare, and early attrition because of such common disorders can have a negative impact on individual and unit operational readiness.
This report documents the frequencies, rates, trends, and distributions of hospitalizations of active component members of the U.S. Army, Navy, Air Force, and Marine Corps during calendar year 2021. Summaries are based on standardized records of hospitalizations at U.S. military and non-military (reimbursed care) medical facilities worldwide. For this report, primary (firstlisted) discharge diagnoses are considered indicative of the primary reasons for hospitalizations; summaries are based on the first 3 digits of the International Classification of Diseases, 10th Revision (ICD-10), used to report primary discharge diagnoses. Hospitalizations not routinely documented with standardized, automated records (e.g., during field training exercises or while shipboard) are not centrally available for health surveillance purposes and thus are not included in this report.
Frequencies, rates, and trends
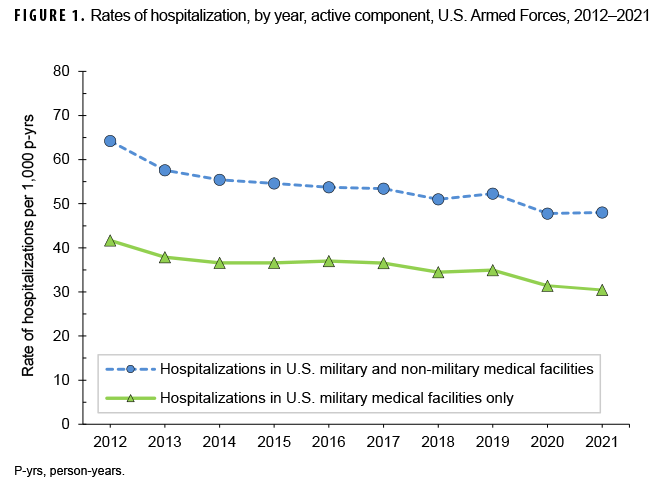
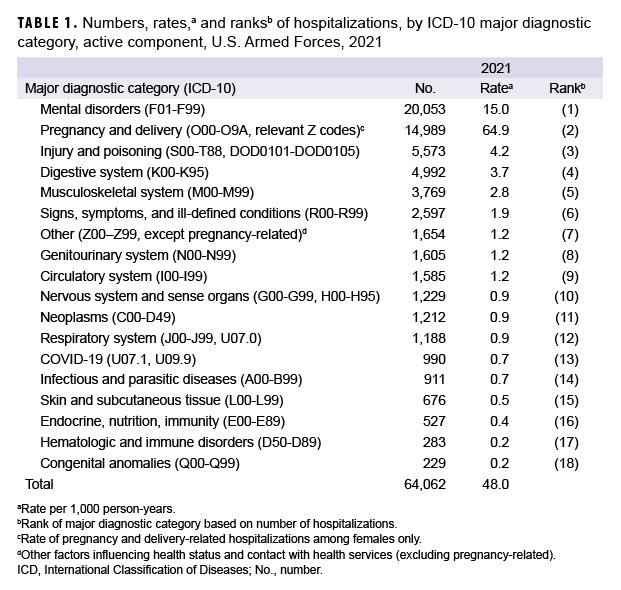
In 2021, there were 64,062 records of hospitalizations of active component members of the U.S. Army, Navy, Air Force, and Marine Corps (Table 1); 36.6% of the hospitalizations were in non-military facilities (data not shown). The annual hospitalization rate (all causes) for 2021 was 48.0 per 1,000 service member person-years (p-yrs) (Table 1). This rate was the second lowest of the years covered in this report (2012–2021), during which rates fell steadily each year until 2019 when the rate (52.3 per 1,000 p-yrs) exceeded that of 2018 (51.0 per 1,000 p-yrs) (Figure 1). The lowest rate of the surveillance period (47.8 per 1,000 p-yrs) was in 2020.
Hospitalizations, by illness and injury categories
In 2021, 4 diagnostic categories accounted for 71.2% of all hospitalizations of active component members: mental health disorders (31.3%), pregnancy- and delivery-related conditions (23.4%), injury/poisoning (8.7%), and digestive system disorders (7.8%) (Table 1). Similar to 2017 and 2019, in 2021 there were more hospitalizations for mental health disorders than for any other major diagnostic category (per ICD-10); 2009 was the last year in which the number of hospitalizations for pregnancy- and delivery-related conditions exceeded the number for mental health disorders (data not shown).
Comparing 2021 to 2017, numbers of hospitalizations decreased in all major categories of illnesses and injuries except for mental health disorders, which increased 10.3% (data not shown). The largest drop in the number of hospitalizations during 2017–2021 was seen in the ICD diagnostic category musculoskeletal system and connective tissue (hospitalization difference, 2017–2021: -1,544; 29.1% decrease) (data not shown).
Hospitalizations, by sex
In 2021, the hospitalization rate (all causes) among female service members was more than 3 times that of male service members (113.0 per 1,000 p-yrs and 33.5 per 1,000 p-yrs, respectively). Excluding pregnancy and delivery, the rate of hospitalizations among female service members (48.1 per 1,000 p-yrs) was 43.6% higher than among male service members (data not shown).
Overall hospitalization rates were higher (i.e., the rate difference [RD] was greater than 1.0 per 1,000 p-yrs) among female than male service members for mental health disorders (female:male, RD: 8.3 per 1,000 p-yrs); genitourinary disorders (RD: 2.6 per 1,000 p-yrs); and neoplasms (RD: 1.3 per 1,000 p-yrs) (data not shown). With the exception of pregnancyand delivery-related conditions, hospitalization rates were relatively similar among male and female service members for the remaining 14 major disease-specific categories (data not shown).
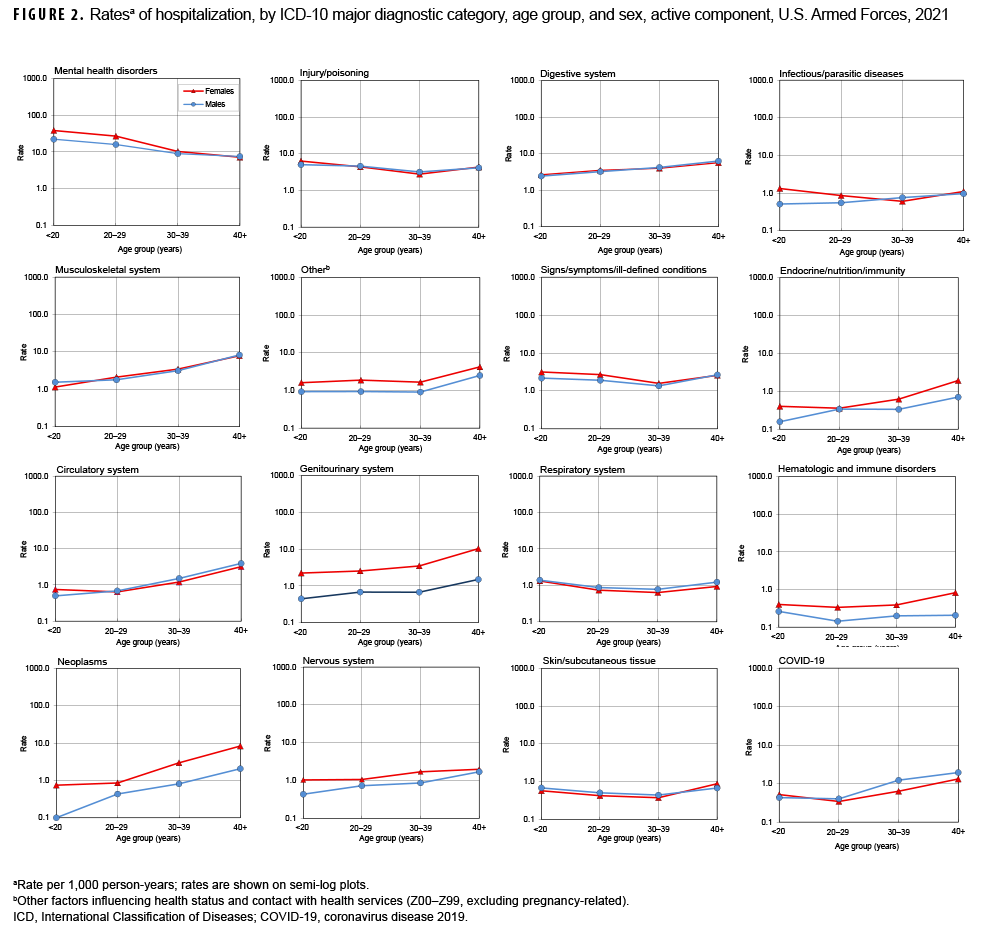
Relationships between age and hospitalization rates varied considerably across illness- and injury-specific categories. For example, among both male and female service members, hospitalization rates generally increased with age for neoplasms, musculoskeletal system/connective tissue disorders, COVID-19, and genitourinary, circulatory, digestive, nervous, and endocrine/nutrition/immunity disorders (Figure 2). Among service members aged 30 or older, there were pronounced differences by sex in the slopes of the rates of neoplasms, and genitourinary, hematologic/immune, and endocrine/nutrition/immunity disorders; the slopes and rates among female service members were notably higher than among male service members in the same age groups. Rates decreased with increasing age for mental health disorders, but were relatively stable across age groups for injury/poisoning, signs/symptoms/illdefined conditions, respiratory system disorders, and infectious/parasitic diseases.
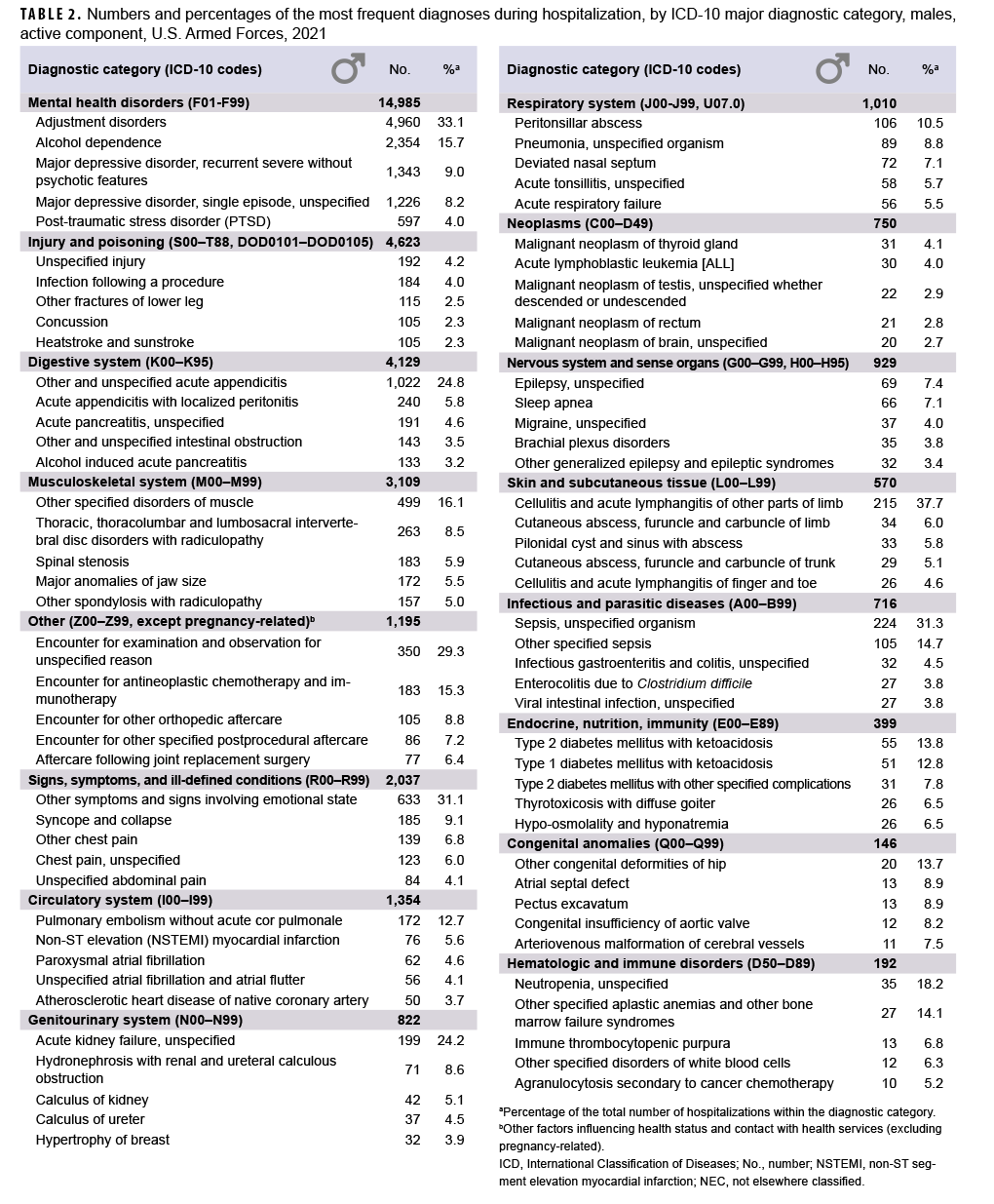
Most frequent diagnoses
In 2021, adjustment disorder was the most frequent discharge diagnosis among male service members (n=4,960) (Table 2). Alcohol dependence (n=2,354), recurrent major depressive disorder [severe without psychotic features] (n=1,343), single episode major depressive disorder [unspecified] (n=1,226), acute appendicitis (n=1,022), other symptoms and signs involving emotional state (n=633), and post-traumatic stress disorder (PTSD) (n=597) were the next 6 most frequent diagnoses in male service members (Table 2).
The most frequent discharge diagnosis among female service members in 2021 was adjustment disorder (n=1,544). Pregnancy and delivery-related conditions represented the next 5 leading causes of hospitalizations among female service members, and this category alone accounted for more than one-half (57.4%) of all hospitalizations of females (Table 3). The top 5 discharge diagnoses in this condition category included post-term (late) pregnancy (n=1,121), abnormality in fetal heart rate and rhythm (n=963), maternal care due to uterine scar from previous surgery (n=833), premature rupture of membranes [onset of labor within 24 hours of rupture] (n=721), and gestational hypertension complicating delivery (n=705). After the top 6 discharge diagnoses described above for female service members, the other leading causes of hospitalizations were recurrent major depressive disorder [severe without psychotic features] (n=563), PTSD (n=501), single episode major depressive disorder [unspecified] (n=459), and alcohol dependence (n=303). Combined, mental health disorder diagnoses accounted for nearly one-fifth (19.4%) of all hospitalizations of female service members.
Injury/poisoning
As in the past, in 2021, injury/poisoning was the third leading cause of hospitalizations of U.S. military members (Table 1). Among male service members, injury/poisoning-related hospitalizations were most often related to unspecified injury, infection following a procedure, other fractures of the lower leg, concussion, or heatstroke/sunstroke (Table 2). Among female service members, injury/poisoning-related hospitalizations were most often related to unspecified injury, poisoning by/adverse effect of/underdosing of other and unspecified antidepressants, infection following a procedure, poisoning by/adverse effect of/underdosing of 4-aminophenol derivatives (e.g., acetaminophen), or other fractures of the lower leg (Table 3).
Durations of hospitalizations
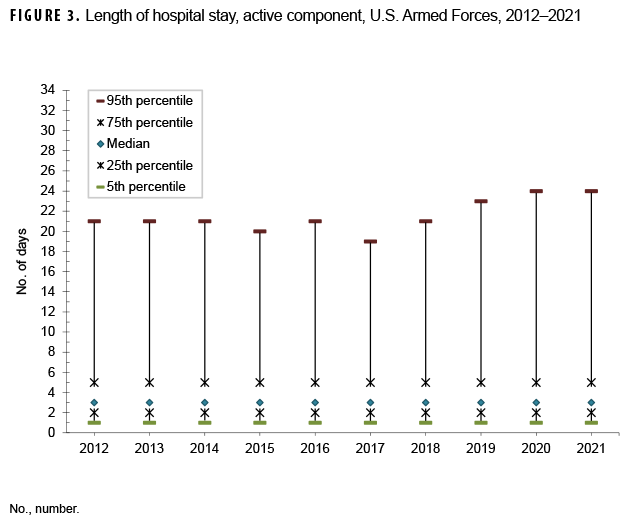
During 2012–2021, the median duration of hospital stays (all causes) remained stable at 3 days (Figure 3). As in previous years, medians and ranges of durations of hospitalizations varied considerably across major diagnostic categories. For example, median lengths of hospitalizations varied from 2 days (e.g., musculoskeletal system disorders; genitourinary system disorders; signs, symptoms, and ill-defined conditions) to 6 days (mental health disorders). For more than one-half of the ICD diagnostic categories, less than 5% of hospitalizations exceeded 10 days, but for 8 categories, 5% of hospitalizations had longer durations: circulatory system disorders (13 days), infectious/parasitic diseases (14 days), COVID-19 (18 days), nervous system/sense organ disorders (19 days), injury/poisoning (19 days), neoplasms (25 days), mental health disorders (30 days), and other non-pregnancy-related factors influencing health status and contact with health services (primarily orthopedic aftercare and rehabilitation following a previous illness or injury) (31 days) (Figure 4).
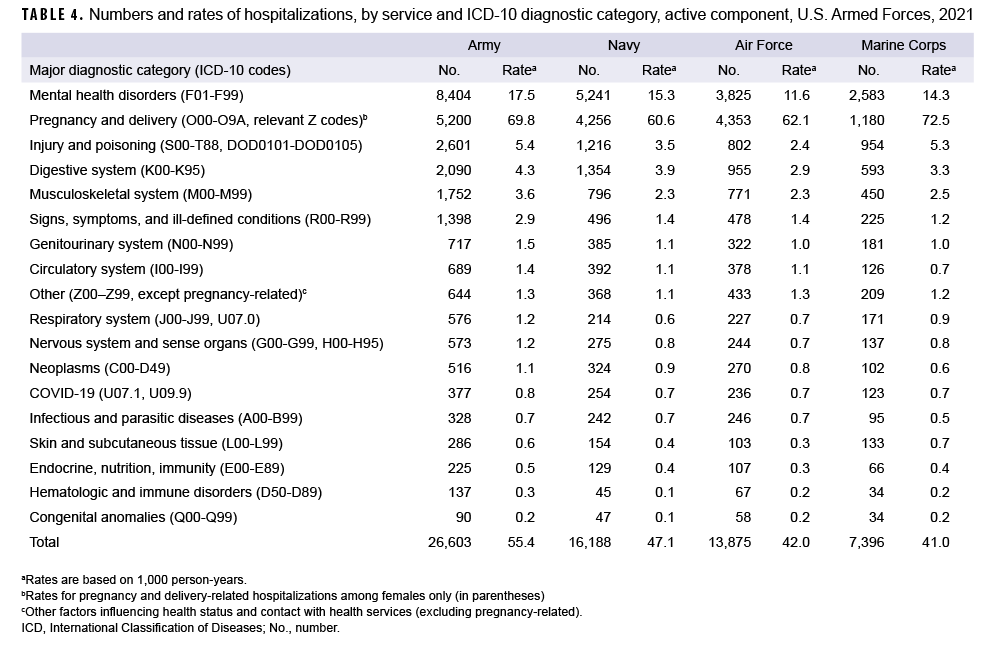
Hospitalizations, by service
Among active component members of the Air Force, pregnancy- and delivery-related conditions accounted for more hospitalizations than any other category of illnesses or injuries; however, among active component members of the Army, Navy, and Marine Corps, mental health disorders were the leading cause of hospitalizations (Table 4). The crude hospitalization rate for mental health disorders among active component Army members (17.5 per 1,000 p-yrs) was higher than among members of all other services. Injury/poisoning was the third leading cause of hospitalizations in the Army and the Marine Corps, and fourth in the Navy and Air Force (Table 4). The hospitalization rate for injury/poisoning was highest among Army (5.4 per 1,000 p-yrs) and Marines Corps members (5.3 per 1,000 p-yrs) and lowest among Air Force members (2.4 per 1,000 p-yrs).
Editorial Comment
The total hospitalization rate for all causes in military and non-military medical facilities among active component members in 2021 was the second lowest rate of the past 10 years. For hospitalizations limited to military facilities, the rate in 2021 was the lowest for the entire period. As in past years, in 2021, mental health disorders, pregnancy- and deliveryrelated conditions, and injury/poisoning accounted for more than half of all hospitalizations of active component members. Adjustment and mood disorders were among the leading causes of hospitalizations among both male and female service members. In recent years, attention at the highest levels of the U.S. military and significant resources have focused on detecting, diagnosing, and treating mental health disorders—especially those related to long and repeated deployments and combat stress. Despite these efforts, crude annual rates of hospitalizations for mental health disorders increased slightly between 2017 and 2021.
The reasons for the recent downturn in the trends for annual numbers of hospitalizations overall and for the slight increase in mental health disorder–related hospitalizations in particular are not clear. It is conceivable that there has been a decline in the impact of combat and peacekeeping operations on overall morbidity among service members since the withdrawal of U.S. forces from Iraq and the official end to combat operations in Afghanistan. The decrease in hospitalizations in 2021 may also have been a consequence of the COVID-19 pandemic, during which elective admissions to hospitals were discouraged and the public health measures of social distancing and use of personal protective equipment may have reduced the incidence of not only infectious diseases but also of injuries. Continued monitoring of hospitalizations and all other health care encounters over time may permit elucidation of the possible reasons for these recent trends.
This summary has certain limitations that should be considered when interpreting the results. For example, the scope of this report is limited to members of the active components of the U.S. Armed Forces. Many reserve component members were hospitalized for illnesses and injuries while serving on active duty in 2021; however, these hospitalizations are not accounted for in this report. Please refer to the snapshot pertaining to the reserve component elsewhere in this issue of the MSMR. In addition, many injury/poisoning-related hospitalizations occur in nonmilitary hospitals. Also, this summary is based on primary (first-listed) discharge diagnoses only; however, in many hospitalized cases, there are multiple underlying conditions. For example, military members who are wounded in combat or injured in motor vehicle accidents may have multiple injuries and complex medical and psychological complications. In such cases, only the first-listed discharge diagnosis would be accounted for in this report. Finally, it should be noted that medical data from sites that were using the new electronic health record for the Military Health System, MHS GENESIS, between July 2017 and October 2019 are not available in the DMSS. These sites include Naval Hospital Oak Harbor, Naval Hospital Bremerton, Air Force Medical Services Fairchild, and Madigan Army Medical Center. Therefore, medical encounter data for individuals seeking care at any of these facilities from July 2017 through October 2019 were not included in the current analysis. Even with these limitations, this report provides useful and informative insights regarding the natures, rates, and distributions of the most serious illnesses and injuries that affect active component military members.