During deployed military operations, initial medical care is provided by military medical personnel stationed within the operational theater, but some injuries and illnesses require medical care outside the theater of operation. In such cases, affected individuals are usually transported to a permanent military medical facility, usually in Europe or the U.S., for definitive diagnosis or care. Because medical evacuations are resource-intensive, they are employed for serious medical conditions, some of which are directly related to participation in, or support of, military operations. Other medical conditions that are unrelated to operational activities but necessitate medical evacuation may be preventable. This report summarizes the nature, numbers, and trends of conditions for which military members were medically evacuated from the U.S. Central Command (CENTCOM) or Africa Central Command (AFRICOM) operations during 2022, with historical comparisons to the previous 4 years.
With completion of the withdrawal of all U.S. military forces from Afghanistan on August 31, 2021, followed by the conclusion of the U.S. combat mission in Iraq on December 9, 2021,1,2 U.S. military operations have been substantially reduced in the CENTCOM area of responsibility (AOR). To sustain counterterrorism operation successes, deployment of forces continues in all AORs, in addition to assistance, advice, and accompaniment of security forces for selected partners, particularly in the CENTCOM and AFRICOM AORs.3 This report only includes medical evacuations from CENTCOM and AFRICOM, without describing any medical evacuations from recent troop deployment to the U.S. European Command (EUCOM), U.S. Indo-Pacific Command (INDOPACOM), or U.S. Southern Command (SOUTHCOM). MSMR has historically reported medical evacuations from CENTCOM due to large numbers of service members deployed for named operations such as Operation Iraqi Freedom, Operation Enduring Freedom, and Operation New Dawn. The AFRICOM AOR was added to this annual report in 2021, due counterterrorism force deployment.3 Future reports may review medical evacuations from other AORs, as required by leadership interest or changing operational tempos.
What are the new findings?
Mental health disorders and injuries constituted the most frequent diagnostic categories for service members medically evacuated in 2022 from U.S. Central Command (CENTCOM) and U.S. Africa Command (AFRICOM). Of the 691 CENTCOM service members and 229 from AFRICOM who were evacuated, hospitalization was required for 245 (35.5%) and 59 (25.8%), respectively. Most service members evacuated from CENTCOM or AFRICOM were returned to full duty status after their post-evacuation hospitalizations or outpatient evaluation.
What is the impact on readiness and force health protection?
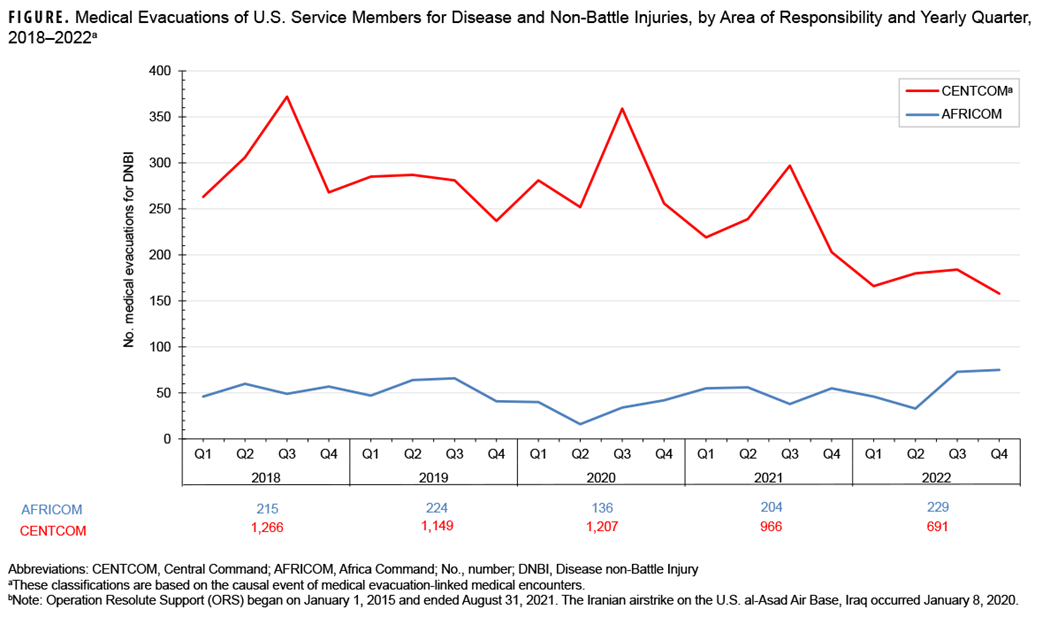
While the number of medical evacuations from CENTCOM declined to the lowest point observed over the last 5 years, during the same period AFRICOM medical evacuations increased to their highest level. These trends correspond with the changes in deployed troop strength within these 2 geographic combatant commands.
Methods
The surveillance population for this analysis includes all members of the active and reserve components of the U.S. Army, Navy, Air Force, and Marine Corps deployed to the CENTCOM or AFRICOM AORs for any length of time from January 1, 2018 through December 31, 2022. Medical evacuations by the U.S. Transportation Command (TRANSCOM) from the CENTCOM or AFRICOM AORs to a medical treatment facility outside the operational theater were assessed from records maintained in the TRANSCOM Regulating and Command & Control Evacuation System (TRAC2ES). Inclusion criteria for this analysis required that any medical evacuee have at least one inpatient or outpatient medical encounter at a permanent military medical facility in the U.S. or Europe within an interval of 5 days before to 10 days after the reported evacuation date. CENTCOM and AFRICOM evacuation data are presented separately.
Medical evacuations were classified by the cause and nature of the precipitating medical condition, based on information in relevant evacuation and medical encounter records. All medical evacuations were classified as “battle injuries” or “non-battle injuries and illnesses,” based on entries in the TRAC2ES evacuation record.
Evacuations due to non-battle injuries and illnesses were further classified into 18 illness/injury categories based on International Classification of Diseases, 9th and 10th Revisions (ICD-9 and ICD-10, respectively) diagnostic codes reported in medical encounter records following evacuation. All records of hospitalizations and ambulatory visits from 5 days before until 10 days after the reported date of each medical evacuation were identified from Defense Medical Surveillance System data. The primary (first-listed) diagnosis for either hospitalization or earliest ambulatory visit after evacuation was used to classify the condition that necessitated the evacuation. If the first-listed diagnostic code specified an external cause of injury (ICD-9 E-code/ICD-10 V-, W-, X-, or Y-code) or an encounter for a condition other than a current illness or injury, the secondary diagnosis specifying illness or injury (ICD-9: 001–999/ICD-10: A00–T88, U07.1, or U09.9) was used. If no secondary diagnosis was provided, or if the secondary diagnosis also was an external cause code, the first-listed diagnostic code of a subsequent encounter was used.
The disposition codes associated with the DMSS medical encounter were used to create a disposition category for each medical evacuation. Inpatient disposition categories include: Returned to duty (code 01), Transferred/discharged to other facility (codes 02–04, 09, 21–28, 43, or 61–66), Died (codes 20, 30, 40–42, 50, or 51), Separated from service (codes 10–15), and Other/unknown. Outpatient disposition categories include: Released without limitation (code 1), Released with work/duty limitation (code 2), Immediate referral (code 4), Sick at home/quarters (codes 3 or S), Admitted/transferred to civilian hospital (codes 7, 9, A–D, or U), Died (codes 8 or G), Discharged home (code F), and Other/unknown.
Results
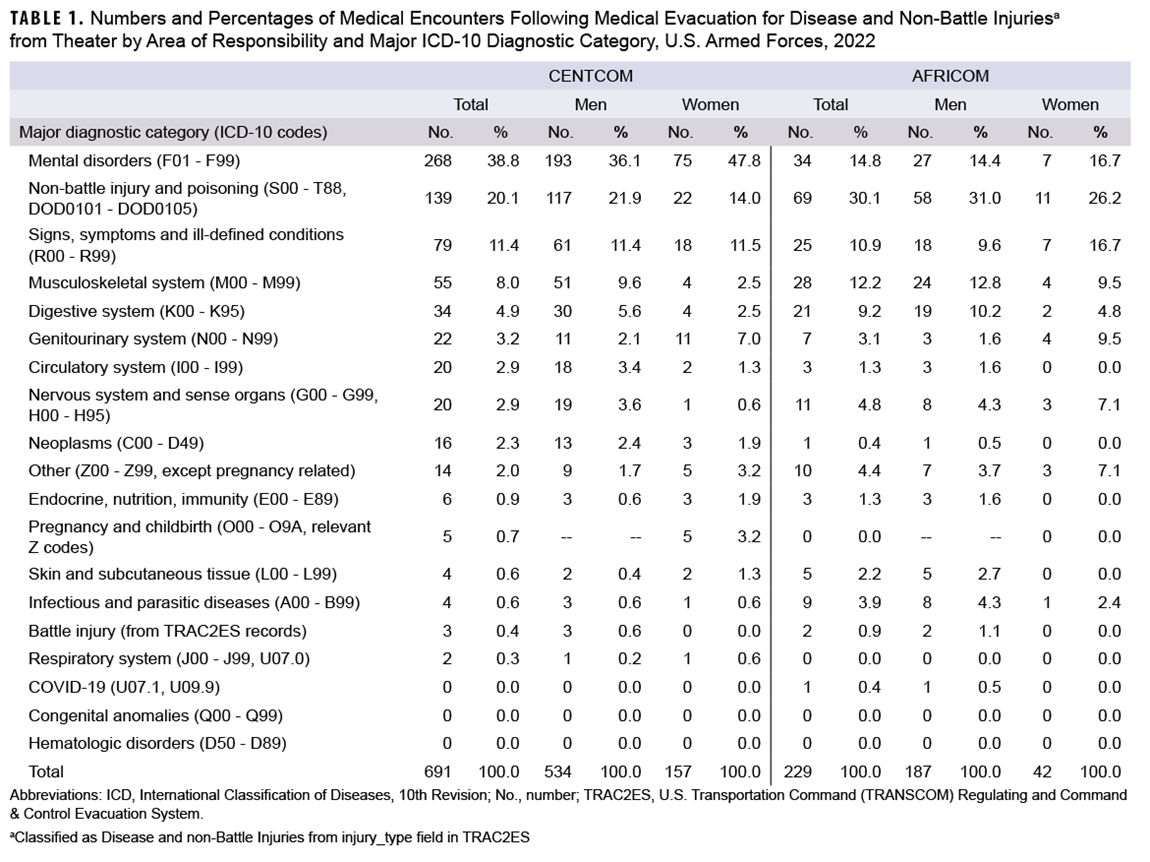
In 2022, 691 service members were medically evacuated from the CENTCOM AOR, while 229 were evacuated from the AFRICOM AOR, with each experiencing at least one subsequent medical encounter at a fixed medical facility outside the operational theater, within the requisite inclusion time frame (Table 1). Mental health disorders accounted for the most medical encounters after a CENTCOM evacuation (n=268; 38.8%), while injury represented the most common diagnostic category after evacuation from AFRICOM (n=69; 30.1%) (Table 1).
Annual CENTCOM medical evacuations attributable to battle injuries remained relatively stable in 2018 (n=57), 2019 (n=59), and 2020 (n=59), subsequently decreasing to near 0 (n=8 in 2021; n=3 in 2022) with the conclusion of major combat operations (data not shown). Annual CENTCOM medical evacuations attributable to non-battle injuries also declined, from 1,266 to 691, during the 2018-2022 surveillance period (Figure). Annual medical evacuations from AFRICOM attributed to battle injuries peaked at six in 2019, then declining to four in 2020 and zero in 2021, with two in 2022 (data not shown). Notably, in 2022 AFRICOM medical evacuations attributable to non-battle injuries and diseases (n=229) exceeded the numbers attributed in the prior four years but remained much lower than CENTCOM (Figure).
Demographic and military characteristics
The leading major diagnostic categories following medical evacuations from CENTCOM and AFRICOM were the same for men and women: mental disorders (from CENTCOM) and non-battle injury (from AFRICOM) (Table 1). Compared to men, female CENTCOM and AFRICOM service members had a higher proportion of medical evacuations for mental health disorders and genitourinary system disorders (Table 1). In contrast, male service members from both AORs had higher proportions of evacuation for injuries, musculoskeletal system disorders, and digestive system conditions.
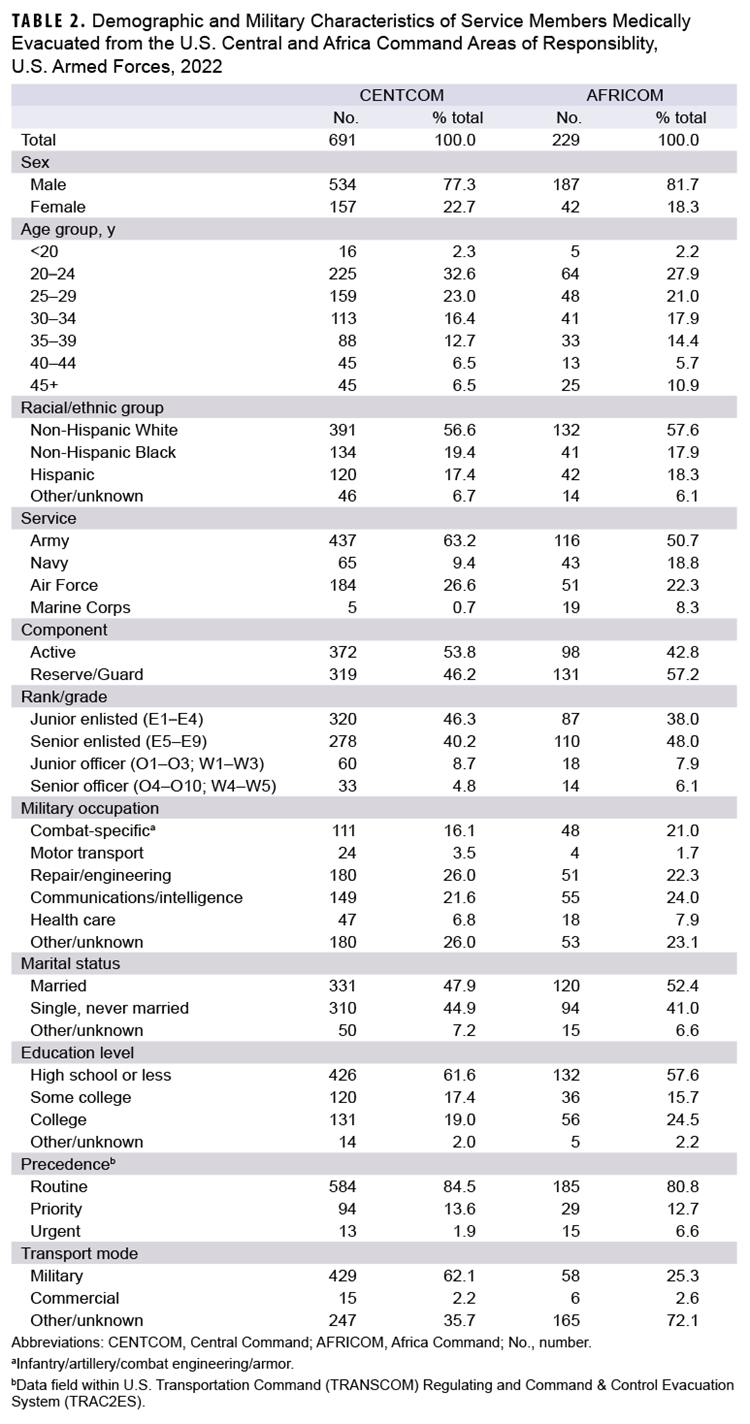
The largest numbers and proportions of CENTCOM and AFRICOM evacuees were non-Hispanic White service members, those aged 20-24 years, members of the Army, and junior and senior enlisted personnel (Table 2). Most CENTCOM (84.5%) and AFRICOM (80.8%) medical evacuations were assigned routine precedence.
Most frequent specific diagnoses
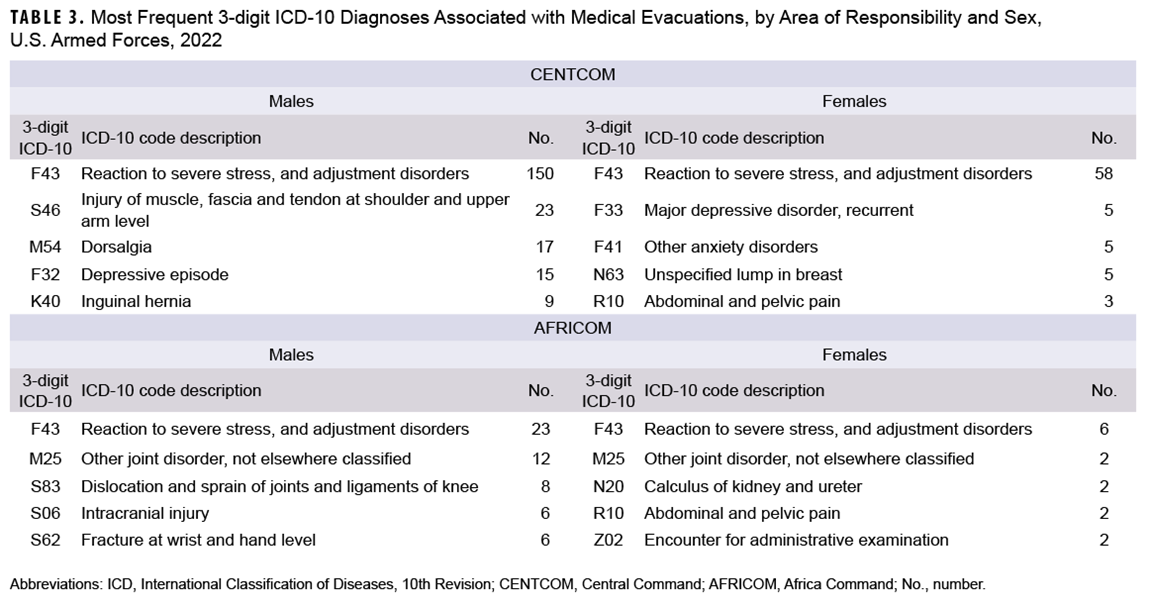
Among men and women in both AORs, the leading 3-digit ICD-10 code for mental health disorders indicated reaction to severe stress and adjustment disorders (F43) (Table 3). This ICD-10 code represented over 75% of mental disorder diagnoses among men and women in both AORs (data not shown).
The proportion of medical encounters for signs, symptoms and ill-defined conditions (R00-R99) accounted for over 10% of all medical evacuations in both AORs (Table 1). The primary diagnoses for the R00-R99 major diagnostic category were not clustered to 1 diagnosis but were diffused throughout this ICD-10 code chapter (data not shown).
Disposition
Hospitalization was required for 245 (35.5%) of CENTCOM (n=691) and 59 (25.8%) of AFRICOM (n=229) medical evacuees in 2022. About four-fifths (82.9% in CENTCOM and 83.1% in AFRICOM) of all service members hospitalized after medical evacuation were returned to duty. A smaller proportion of CENTCOM medical evacuees with subsequent outpatient encounters were released without limitation (69.5%) compared to AFRICOM evacuees (84.1%) (data not shown).
Discussion
Only 5 (0.3%) medical evacuations from CENTCOM (n=3) and AFRICOM (n=2) in 2022 were associated with battle injuries in the TRAC2ES records. While CENTCOM medical evacuations attributable to non-battle injuries declined to the lowest number observed in the last 5 years, during the same period AFRICOM non-battle injury medical evacuations increased to their highest level. These trends coincide with the drawdown in forces from CENTCOM and reestablishment of persistent military forces throughout East Africa.3
The leading diagnoses of AFRICOM non-battle injuries were not clustered around any specific ICD-10 code but distributed among diagnoses such as dislocation and sprain of joints and knee ligaments, intracranial injuries, and wrist or hand fractures. This heterogeneity of injury type may be due to the large proportion resulting from occupational hazards in the deployed environment. Classification by cause of injury rather than affected body system may be more appropriate for this population.
The proportion of CENTCOM medical evacuations in 2022 attributed to mental health disorders (38.8%; n=268) represents a continued increase from the proportions reported in 2021 (33.5%; n=323), 2020 (27.2%; n=327), and 2019 (27.1%; n=308). These rates of medical evacuation due mental health disorders are also considerably higher than the proportion (11.6%; n=5,892) described by a MSMR report examining evacuations from Iraq during a 9-year period between 2003 and 2011.4-7
Several important limitations should be considered when interpreting these results. Demographic data for the deployed population, i.e. person-time for individuals eligible for medical evacuation, are not readily available. A Government Accountability Office finding that the DOD does not maintain complete data to allow monitoring of personnel tempo limits assessment of the amount of time service members are deployed or assigned for service away from home for other events.8 The lack of deployed individual person-time precludes calculation of stratified and overall rates for medical evacuations.
Most causes of medical evacuations were estimated for this report from primary (first-listed) diagnoses in DMSS recorded during hospitalizations or initial outpatient encounters following evacuation. Diagnoses recorded in theater through the Theater Medical Data Store are not reflected in this analysis. In some cases, clinical evaluations at fixed medical treatment facilities following medical evacuation may have ruled out serious conditions clinically suspected while in theater, resulting in possible misclassification errors. Battle injuries rely on proper classification in the TRAC2ES system. Misclassification errors may occur, and given the small number of battle injuries, any misclassification will have an outsized effect.
As troop drawdown continues in CENTCOM, increasing non-battle injuries among AFRICOM medical evacuees may pose challenges due to AFRICOM’s particular logistical conditions, including extreme force dispersion, long distances for medical evacuation, and relatively few medical assets. While the substantial number of mental disorders following evacuation may indicate ongoing need for mental health services or reexamination of the pre-deployment screening process, the large proportion of service members evacuated with injury and musculoskeletal disorders from the AFRICOM AOR constitutes a major potentially preventable risk that degrades the readiness of the deployed force.
References
- White House Briefing Room. Remarks by President Biden on the End of the War in Afghanistan. August 31, 2021. Accessed March 24, 2022. https://www.whitehouse.gov/briefing-room/speeches-remarks/2021/08/31/remarks-by-president-biden-on-the-end-of-the-war-in-afghanistan
- Kullab, Samya. US formally ends combat mission in Iraq. Military Times. December 9, 2021. Accessed March 24, 2022. https://www.militarytimes.com/news/your-military/2021/12/09/us-formally-ends-combat-mission-in-iraq
- White House Briefing Room. Letter to the Speaker of the House and President Pro Tempore of the Senate Regarding the War Powers Report. December 8, 2022. Accessed July 5, 2023. https://www.whitehouse.gov/briefing-room/statements-releases/2022/12/08/letter-to-the-speaker-of-the-house-and-president-pro-tempore-of-the-senate-regarding-the-war-powers-report-4
- Armed Forces Health Surveillance Division. Medical evacuations out of the U.S. Central Command, active and reserve components, U.S. Armed Forces, 2019. MSMR. 2020;27(5):27-32.
- Armed Forces Health Surveillance Division. Medical evacuations out of the U.S. Central Command, active and reserve components, U.S. Armed Forces, 2020. MSMR. 2021;28(5):28-33.
- Armed Forces Health Surveillance Division. Medical evacuations out of the U.S. Central and U.S. Africa Commands, active and reserve components, U.S. Armed Forces, 2021. MSMR. 2022; 29(6):27-33.
- Armed Forces Health Surveillance Center. Medical evacuations from Operation Iraqi Freedom/Operation New Dawn, active and reserve components, U.S. Armed Forces, 2003–2011. MSMR. 2012;19(2):18-21.
- United States Government Accountability Office. Report to Congressional Committees. GAO-18-253, Military Readiness: Clear Policy and Reliable Data Would Help DOD Better Manage Service Members’ Time Away from Home. April 2018. Accessed July 5, 2023. https://www.gao.gov/assets/gao-18-253.pdf