What Are the New Findings?
Among a group of service members whose duties involved frequent weapons training and exposure to lead, a focused effort to reduce exposures to lead was associated with a reduction in BLLs among the exposed service members.
What Is the Impact on Readiness and Force Health Protection?
This article emphasizes the special occupational hazards associated with lead related to firing ranges, the general nature of mitigation measures, and the health effects that are associated with lead toxicity. Awareness of these issues and surveillance of service members at risk of lead toxicity will enable leaders and public health officials to act to prevent adverse health effects among those who are commonly exposed.
Abstract
This report describes the results of testing for blood lead levels (BLLs) among special operations forces at a single installation in Germany where occupational exposures to lead were associated with use of a firing range. After recognition of elevated BLLs in some service members who used the firing range, a detailed industrial hygiene confirmation of lead exposures prompted mitigation measures undertaken by command authorities, facilities management, public health, and clinical occupational medicine. To assess the impact of the mitigation efforts, this study retrieved the results of all BLLs performed between 1 January 2016 and 30 Sept. 2018 among SOF soldiers enrolled in an Occupational Safety and Health Administration (OSHA)-required medical surveillance program for lead exposure. Mitigation steps were taken during July–Sept. 2017. BLLs from the periods before and after the mitigation efforts were compared. Among the 57 individuals who had levels measured both before and after the mitigation period, the range of BLL values fell from a range of 1–35 μg/dL to a range of 1–15 μg/dL. The number of individuals who had BLLs of greater than 20 μg/dL fell from 9 before, to 0 after the mitigation period. The various types of mitigation steps useful in reducing firing range-related lead exposure are described.
Background
Use of indoor and outdoor firing ranges is a well-known source of airborne lead exposure for Special Operations Forces (SOF) populations and can result in subsequent elevated blood lead levels (BLL). This source of lead exposure can be especially problematic during high volume training and/or use of inadequately ventilated firing areas.1–3 Lead toxicity can have a significant negative impact on military readiness4 and can degrade physical and psychological performance, especially in this population of specialized soldiers. Symptoms associated with elevated BLLs include abdominal distress, depression, distractibility, forgetfulness, irritability, weakness, fatigue, memory loss, pain, and/or paresthesias in hands and/or feet, and headaches.5 Prolonged lead exposure can cause hematologic disorders, hypertension, degradation of the central and peripheral nervous systems, renal disease, miscarriages, and male fertility complications.6
Important sources of lead exposure include fine particulates from primers and projectile fragments from ammunition as well as primers used in pyrotechnics and explosives. Such lead exposures are especially concerning in high-volume training and/or enclosed or inadequately ventilated firing areas. The major routes of lead internalization are inhalation and ingestion. The primary cause of inhalation exposure occurs during the process of firing a weapon when fine, aerosolized lead particulates escape from the chamber, port, and barrel of a weapon. Many of these particulates can be inhaled during weapons' firing. Lead particulates that are not inhaled will eventually fall to the ground or adhere to bodies, clothing, and equipment. Additional lead particulates are generated when lead projectiles strike hardened targets or the firing range backstop. The accumulation of these lead particulates on the ground, backstop, bodies, clothing, and equipment are sources of secondary inhalation exposure. Disruption and re-aerosolization of accumulated lead particulates occur as a result of movements of shooters, projectiles striking the backstop, the use of explosives and pyrotechnics, cleaning of firing ranges and equipment, and the changing of contaminated clothing. The primary sources of lead ingestion exposure are particulates that are adherent to hands and that contaminate hydration sources. Ingestion occurs if lead has not been washed from the hands before eating, smoking, or using smokeless tobacco, or if it is not removed from a hydration source before drinking.
In response to the risks associated with occupational lead exposure, the Occupational Safety and Health Administration (OSHA) and the Department of Defense (DOD) have set guidelines regarding acceptable levels for blood lead and for medical surveillance of workers exposed to lead. Medical surveillance is critical for documenting effects of lead exposure and providing employers and employees with appropriate medical guidance. For workers above certain lead exposure levels, OSHA requires enrollment in a medical surveillance program with initial and periodic exams to track and review BLLs.7 DOD lead exposure surveillance standards comply with those of OSHA, yet are more stringent, particularly with regard to standards of when an employee is to be removed from and returned to lead work.8
This current report describes a SOF population at a single installation in Germany with exposure to airborne lead, resultant elevated BLLs, and the successful cooperative efforts that resulted in a significant overall decrease in that population's BLLs. As early as 2000, Mancuso et al. recognized that this unique population had elevated BLLS believed to be primarily due to high-volume firing in enclosed or partially covered ranges.1 Several groups undertook efforts between 2016 and 2017 to decrease this exposure, including industrial hygiene (IH), facilities (range) management, unit command, public health, and clinical occupational medicine.
An IH assessment of unit firing ranges in 2016 revealed that the soldiers' exposure to airborne lead was the equivalent of breathing lead concentrations of 190 to 250 μg/m3 for 8 hours. This exposure is up to 5 times the OSHA permissible exposure limit of an 8-hour time-weighted average (TWA) of 50 μg/m3 and more than 8 times the OSHA action level of an 8-hour TWA of 30 μg/m3.7 Informed by these findings, IH made key recommendations to remediate these exposures. Based on these recommendations, facilities management replaced contaminated sand and synthetic backstops, exchanged some sand backstops with synthetic backstops, and limited 1 firing range with a sand backstop to low-volume firing exercises only. Unit leadership implemented additional risk mitigation measures that included enforcing more stringent removal of any soldier with a single BLL of ≥20 μg/dL from live weapons training, as well as requiring the use of unit laundering facilities and lead abatement hand wipes after firing. Public health and occupational medicine personnel advocated for the implementation of IH recommendations and provided lead exposure education to SOF personnel and leadership during site visits and clinical encounters.
Methods
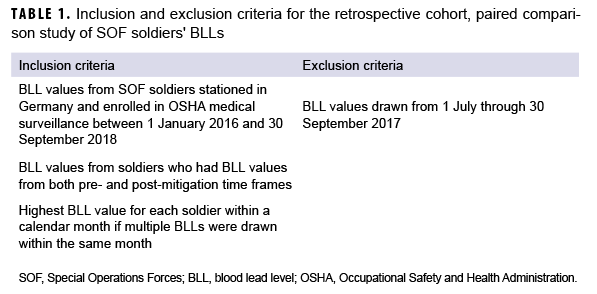
Venous BLLs measured in 130 SOF soldiers enrolled in OSHA-required medical surveillance at 1 installation in Germany between 1 January 2016 and 30 Sept. 2018 were reviewed. To allow for a paired comparison, only the BLLs of SOF soldiers with results from the pre-mitigation and post-mitigation time frames were included in this analysis (Table 1). Laboratory results of venous BLLs were collected from electronic medical records in Armed Forces Health Longitudinal Technology Application (AHLTA). For purposes of this study, to address inconsistent frequency of lab draws, only 1 BLL value was included per calendar month for any individual. If multiple BLL samples were drawn from an individual during a single month, the highest recorded value was included and all others were excluded (Table 1). Each BLL value was recorded in units of micrograms of lead per deciliter of blood (μg/dL). All BLL values were reported in whole numbers; any BLL value 1 μg/dL or less was recorded as 1 μg/dL.
Descriptive statistical data analysis was performed using QI Macros Statistical Process Control software add-in version 2018.07 (KnowWare International, Inc.) for Microsoft Excel. The resulting BLL data were categorized as pre-mitigation or post-mitigation based on the timing of the blood draw. Three months of data immediately after mitigation (July–Sept. 2017; 60 BLL samples) were excluded to avoid a potential positive bias; this period is consistent with the half-life of lead in blood, 36 ± 5 days.6 Statistical analysis was performed with R version 3.6.1 (2019, R Core Team, R Foundation for Statistical Computing). Since an individual's BLLs are temporally interdependent and there was inconsistent follow-up, specialized statistical techniques were required. To overcome the interdependence problem, 1 million resampling simulations were performed. In each simulation, a single BLL measurement was randomly sampled from each of the pre- and post-mitigation periods for each individual, thereby ensuring the independence of observations within each simulation. For each simulation, the ratio of post-mitigation over pre-mitigation BLLs was calculated. The proportion exceeding 1 is the p-value for this nonparametric, simulation-based approach, which was similarly used to estimate the effect size.
Results
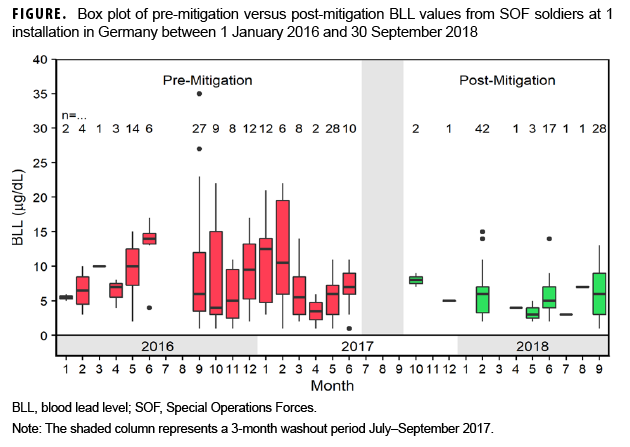
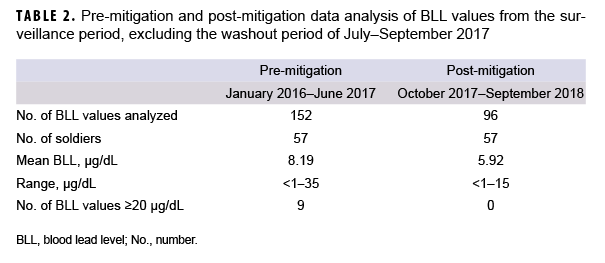
Between 1 Jan. 2016 and 30 Sept. 2018, a total of 473 BLL samples were drawn from 130 individuals of a SOF company stationed in Germany (Figure). The number of samples drawn per individual during the 33-month surveillance period ranged from 1–11, while the number of samples drawn from the company per month varied from 0–58. For the 57 individuals with both pre- and post-mitigation samples, the BLL values fell from a range of 1–35 μg/dL during the pre-mitigation interval to a range of 1–15 μg/dL post-mitigation (Table 2). The number of individuals with a BLL of ≥20 μg/dL (the company action level for removal from lead exposure) before mitigation efforts was 9; after mitigation, there were no individuals with a BLL at or above the action level.
A 1 million trial, nonparametric simulation (on the ranks of BLLs within each individual, not on the actual BLL values) determined that post-mitigation BLLs were lower than pre-mitigation BLLs (p=.02). The corresponding simulation on the actual BLL values was consistent with this result, although not statistically significant (p=.05). Post-mitigation BLLs were on average 87% of the pre-mitigation value (95% confidence interval: 75%–102%).
Editorial Comment
This study demonstrates the effectiveness of a multidisciplinary approach to providing a training environment that is both realistic and safe for soldiers who participate in frequent live-fire small arms training. The reduction of the mean BLLs within this population demonstrates an association with the mitigation strategies recommended by IH and implemented by facilities management and the unit command. The following measures were carried out: replacing sand backstops with synthetic backstops; limiting types of firearms on firing ranges with sand backstops; reducing the BLL threshold to a single result of 20 μg/dL for removing a soldier from lead exposure; and enforcing the use of unit laundering facilities and lead abatement hand wipes after firing.
Additional actions that may be helpful in lead exposure mitigation include but are not limited to the following: replacement of lead ammunition with lead-free ammunition such as SINTOX; improvement of range ventilation systems; provision of hand-washing facilities and running water at every firing range; provision of lead abatement hand wipes and lead-specific soap and laundry detergents; enforcement of respiratory protection measures during range cleanup; and provision of "sweep" materials and enforcement of their use. Ongoing IH monitoring at these firing ranges (annually or more frequently) and continued medical surveillance are crucial tools for unit leadership, medical providers, and the individual in order to assure range safety, optimal soldier readiness, and treatment recommendations.
Several limitations to the current analysis merit mention. Although the exposures focused on in this report are at the same ranges as discussed by Mancuso et al.,1 it is unknown to the authors if there were any soldiers who were included in both studies (i.e., 2000–2005 and 2016–2018). It is also unknown to the authors of any engineering controls that were implemented from 2005 through July 2017. The data presented here were derived from a very active, fluid population. Accordingly, not all individuals were available at each recommended testing interval (baseline and quarterly). Some individuals did not receive each test, for reasons such as deployments, training, or permanent moves. The personnel dates of assignment to this unit, previous unit assignments and thus previous lead exposures are unknown to the authors. A true washout period of 5 half-lives without further lead exposure was precluded by the necessity of continued training on other available firing ranges. Because of the medical requirements of certain schools and the request of unit-assigned medical personnel, testing occurred more frequently than quarterly for some soldiers; this led to a wide range of sample sizes per individual (1–11) and a wide variance in the number of tests drawn from this population per month (0–58). Because these data were analyzed and considered at the population level and not the individual level, they present a strong association; however, this association cannot be considered causal. Ranked BLLs were found to decrease, and this change was statistically significant; however, results of a similar analysis on the actual BLLs were consistent but not statistically significant. Small sample size and the limited number of paired samples may have contributed to limited findings, as well. Furthermore, follow-up IH sampling is required to evaluate the effects of the newly implemented engineering controls on lead exposure at these firing ranges.
Overexposure to lead in the U.S. military is an ongoing risk, especially in populations that participate in frequent live-fire small arms training within enclosed spaces. Service members whose mission requires frequent live-fire small arms training may be at highest risk of decreased readiness if exposed to lead. While mild overexposure to lead and subsequent low-level toxicity may not affect a service member's deployability, some of the subtle symptoms (e.g., decreased attention, slower cognition, or decreased reaction time) could have an adverse impact on an affected individual's physical and psychological performance.9 Family members, particularly children, are additionally at risk of exposure and subsequent medical concerns if the lead particulates are not removed from the bodies, equipment, and clothing of soldiers before entering their personal vehicles or their homes.
Author affiliations: U.S. Army Medical Department Activity Bavaria, Department of Preventive Medicine (MAJ Hyten, Ms. Slusher, LTC Mease); Madigan Army Medical Center, Joint Base Lewis-McChord, WA (Dr. Colburn, Ms. Slusher, LTC Mease).
Acknowledgements: MAJ Philip Castaneda for consultation and assistance with the Special Forces Soldier and Unit; COL (Ret) Mark D. Swofford, PhD, MHA for leadership and consultation; CSM Kevin P. Dorsh for unit coordination and advocacy; Paul G. Sweeney, CIH for Industrial Hygiene support and consultation; and Ashby Payne, BSN, MPA, for Public Health Nursing support and consultation.
Financial support: All work described herein was performed as part of paid regular duties as part of employment by the U.S. Government.
Conflict of interest: None.
References
- Mancuso JD, McCoy J, Pelka B, Kahn PJ, Gaydos JC. The challenge of controlling lead and silica exposures from firing ranges in a special operations force. Mil Med. 2008;173(2):182–186.
- Laidlaw MAS, Filippelli G, Mielke H, Gulson B, Ball AS. Lead exposure at firing ranges - a review. Environ Health, 2017;16(1):34.
- Beauchman C, Page E, Alarcon WA, Calvert GM, Methner M, Schoonover TM. Indoor firing ranges and elevated blood lead levels - United States, 2002–2013. MMWR Morb Mortal Wkly Rep. 2014;63(16):347–351.
- Greenberg N, Frimer R, Meyer R, Derazne E, Chodick G. Lead exposure in military outdoor firing ranges. Mil Med. 2016;181(9):1121–1126.
- National Institute for Occupational Safety and Health (NIOSH). Health problems caused by lead. Accessed 17 Sept. 2018. https://www.cdc.gov/niosh/topics/lead/health.html.
- Wani AL, Ara A, Usmani JA. Lead toxicity: a review. Interdiscip Toxicol. 2015;8(2):55–64.
- U.S. Department of Labor. Occupational Safety and Health Administration. Standard 1910.1025. Lead. Accessed 17 Sept. 2018. https://www.osha.gov/laws-regs/regulations/standardnumber/1910/1910.1025.
- Office of the Under Secretary of Defense for Acquisition and Sustainment. Occupational Medical Examinations and Surveillance Manual. DoD 6055.05-M (2017). Accessed 14 November 2018. http://www.esd.whs.mil/Portals/54/Documents/DD/issuances/dodm/605505mp.pdf.
- Todd AC, Wetmur JG, Moline JM, Godbold JH, Levin SM, Landrigan PJ. Unraveling the chronic toxicity of lead: an essential priority for environmental health. Environ Health Perspect. 1996;104(suppl 1):141–146.