Frequently Asked Questions about measles outbreaks and MMR vaccine policy and recommendations
Measles

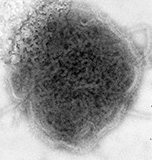
Measles is a highly contagious acute viral respiratory illness caused by a single-stranded, enveloped RNA virus with 1 serotype. Humans are the only natural hosts of measles virus.
Transmission of the measles virus is through direct contact with infectious droplets or by airborne spread when an infected person breathes, coughs, or sneezes. Measles virus can remain infectious in the air for up to two hours after an infected person leaves an area.
Clinical features include a prodrome marked by high fever followed by the onset of cough, runny nose, and red, watery eyes (conjunctivitis). Koplik spots may be seen on mucous membranes in the mouth; these lesions present as blue and white spots on bright red background and appear a few days before and after the measles rash. The characteristic measles rash appears as maculopapular lesions that start on the head and gradually proceed down the body over 5-6 days.
Complications develop in approximately 30% of measles cases, which are most common in children younger than 5 years and adults 20 years and older. Complications include ear infections, diarrhea, pneumonia, or encephalitis (brain inflammation), and rarely death.
There is no cure for measles. Treatment is symptomatic and supportive.
Mumps
Mumps is an acute viral illness caused by an enveloped RNA virus that belongs to the genus Rubulavirus, in the family Paramyxoviridae. Humans are the only natural hosts for mumps virus, which is usually spread by respiratory droplets, saliva, or contact with contaminated fomites. The incubation period of mumps averages 16–18 days, with a range of about 2–4 weeks.
Mumps infection may present with primarily respiratory symptoms or may be asymptomatic. However, clinical features of mumps usually include unilateral or bilateral, parotitis, with single or multiple salivary glands affected. Parotitis occurs within the first 2 days and may first be noted as earache and tenderness on palpation of the angle of the jaw. Symptoms tend to decrease after 1 week and usually resolve after 10 days. Nonspecific prodromal symptoms may precede parotitis by several days, including low-grade fever which may last three to four days, myalgia, anorexia, malaise, and headache.
Complications of mump infections are more likely to be serious when adults are infected. Complications of mumps can include meningitis (in up to 15% of cases), orchitis, and deafness. Very rarely, mumps can cause encephalitis and permanent neurological damage.
Rubella
 Rubella, also called German measles, is a contagious viral infection caused by rubella virus. Humans are the only natural hosts of rubella virus, which is transmitted through person-to-person contact or droplets shed from the respiratory secretions of infected people. People may shed virus from 7 days before the onset of the rash to approximately 5–7 days after rash onset. Transmission from mother to fetus can also occur, with the highest risk of congenital rubella syndrome if infection occurs in the first trimester. Infants with CRS can transmit virus for up to 1 year after birth.
Rubella, also called German measles, is a contagious viral infection caused by rubella virus. Humans are the only natural hosts of rubella virus, which is transmitted through person-to-person contact or droplets shed from the respiratory secretions of infected people. People may shed virus from 7 days before the onset of the rash to approximately 5–7 days after rash onset. Transmission from mother to fetus can also occur, with the highest risk of congenital rubella syndrome if infection occurs in the first trimester. Infants with CRS can transmit virus for up to 1 year after birth.
Symptoms of rubella are often mild, and up to 50% of infections may be subclinical or inapparent. Rubella usually presents as a nonspecific, maculopapular, generalized rash that lasts ≤3 days with generalized lymphadenopathy. Rash may be preceded by low-grade fever, malaise, anorexia, mild conjunctivitis, runny nose, and sore throat. Adolescents and adults, especially women, can also present with transient arthritis. Infection during early pregnancy can lead to miscarriage, fetal death, or the fetus can develop Congenital Rubella Syndrome, which can affect virtually all organ systems, with deafness being the most common outcome. Up to 85% of infants are affected if infection occurs during the first trimester of pregnancy.
Complications of rubella are not common, and generally occur more often in adults than in children. Arthralgia or arthritis may occur in up to 70% of adult women who contract rubella, and tend to occur about the same time or shortly after appearance of the rash, lasting for up to 1 month. Additional complications that can occur are encephalitis, orchitis, neuritis, and a late syndrome of progressive panencephalitis. Complications that do occur more often in children than adults are hemorrhagic manifestations (approximately one per 3,000 cases) that may be secondary to low platelets and vascular damage, with thrombocytopenic purpura being the most common manifestation. Gastrointestinal, cerebral, or intrarenal hemorrhage may occur. Effects may last from days to months, and most patients recover.
M-M-R®II is a live-virus vaccine which includes antigens for measles, mumps, and rubella, licensed for persons 12 months and older. Two doses of MMR vaccine are routinely recommended for children, starting with the first dose at age 12 through 15 months and the second dose at age 4 through 6 years before school entry. Children can receive the second dose earlier as long as it is at least 28 days after the first dose.
Teens and adults should also be up to date on MMR vaccinations. MMR vaccination is especially important for:
- Students at post-high school educational institutions
- International travelers
- Healthcare professionals
- Women of childbearing age who are not pregnant
- People who care for or are around immunocompromised people
- People living with HIV without evidence of severe immunosuppression
After vaccination, it is not necessary to test patients for antibodies to confirm immunity.
ProQuad® (MMRV) is a live-virus combination vaccine which includes antigens for measles, mumps, rubella, and varicella. ProQuad® is licensed for children 12 months through 12 years of age. If MMRV vaccine is used, at least 3 months should elapse between doses of varicella-containing vaccine.
You will find below all of the resources you will need about the measles-mumps-rubella vaccine. More will be added as they are published or released.
| Information Paper |
Date |
MMR Infections and the MMR Vaccine
|
March 21, 2023 |
Cold Chain Management of MMR Vaccine
|
Jan. 31, 2023 |
| Standing Orders |
Date |
Measles Mumps Rubella Vaccine (Pediatric)
|
May 15, 2023 |
Measles Mumps Rubella Varicella Vaccine (Pediatric)
|
May 15, 2023 |
Measles Mumps Rubella Vaccine (Adult)
|
May 17, 2023 |
| Vaccine Information Statements (VIS) |
Date |
MMR Vaccine: What You Need to Know
|
Aug. 6, 2021 |
MMRV Vaccine: What You Need to Know
|
Aug. 6, 2021 |
| Manufacturer Package Inserts |
Date |
M-M-R II
|
Aug. 21, 2023 |
PRIORIX
|
June 3, 2022 |
ProQuad (MMRV) (frozen)
|
Aug. 21, 2023
|
| Advisory Committee on Immunization Practices (ACIP) Recommendations |
Date |
MMR Vaccine
|
Nov. 18, 2022 |
MMRV Vaccine
|
May 7, 2010 |